The mass death of immune cells 10 months after Covid infection
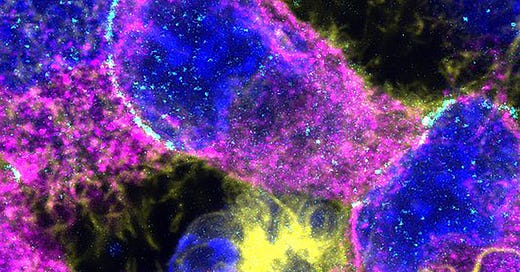
Upon this antigen I shall build my church
Also before I even start writing anything, and in very big letters because I know some people have difficulty accepting certain facts.
This study was done between May and August 2020, there was no mRNA in the world, no vaccines, and no reinfections.
Unless the patients and samples in this study are both time travelers, yeah, this is mostly the virus.
Differential decline of SARS-CoV-2-specific antibody levels, innate and adaptive immune cells, and shift of Th1/inflammatory to Th2 serum cytokine levels long after first COVID-19
It has been known that acute and severe SARS-CoV-2 infection are able to induce long-term changes in many functions of the body, from cell metabolism to organ function itself, but so far it is not known even infections cause long-lasting changes. Here they analyzed the samples of 133 patients at 2 time points. 10 weeks after infection, and as a first ,10 months.
Since antibody levels became the way protection is measured, this was the first step. Antibody levels against the spike (S), receptor-binding domain (RBD), and nucleocapsid (NC) proteins significantly decreased between 10 weeks and 10 months after infection. Specifically, S and RBD antibodies declined below the detection limit in almost 18% and over 80% of subjects, respectively, at 10 months. Conversely, anti-NC antibodies remained above the detection limit in all subjects, indicating a different kinetic decline compared to S and RBD antibodies.
Given there was a distinct pattern between the antibody decline between these 3 proteins, they further analyzed it and divided the patients into 3 groups. This will be very important later.
Group 1 had a low to moderate decrease in Nucleocapsid levels
Group 2 showed a high decrease in N but a low decrease in Spike antibody levels
Group 3 had a high decrease in both N and S.
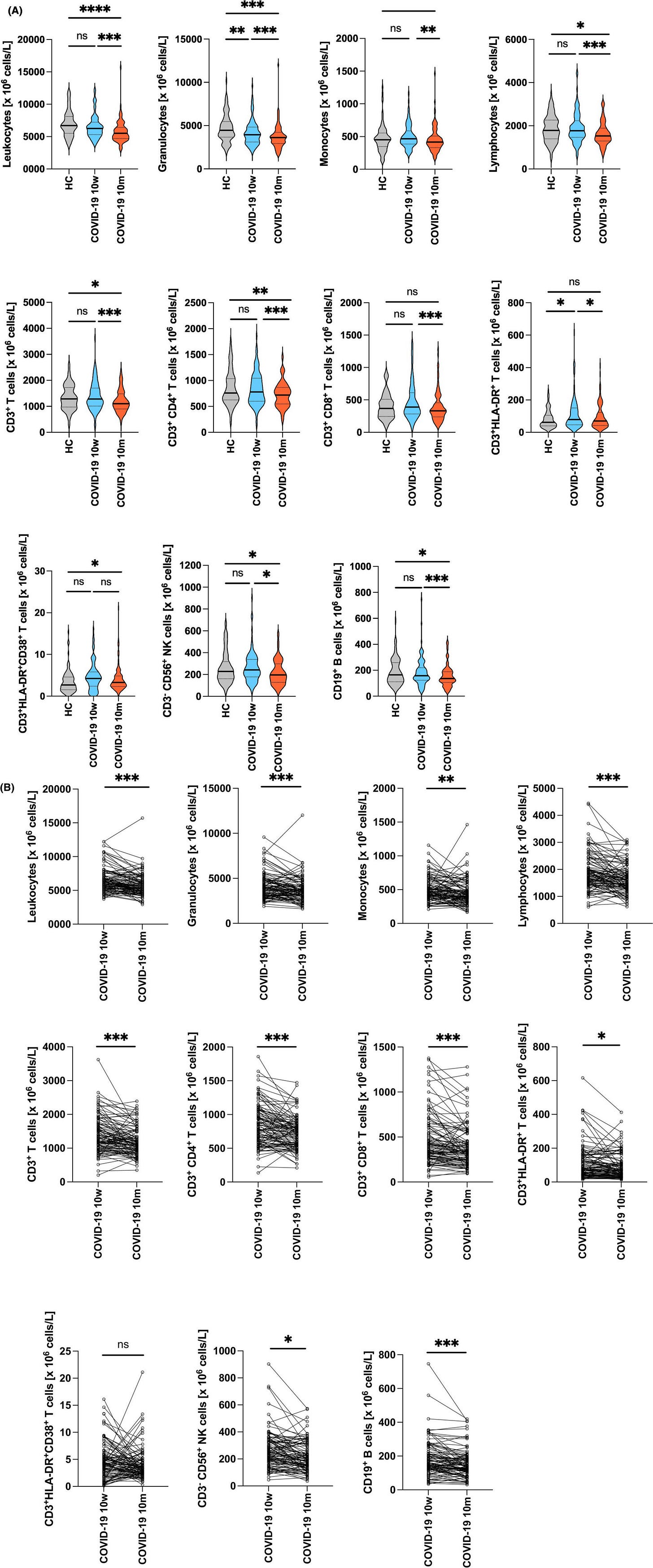
Leukocyte (immune cells) reduction as late as 10 months after infection
As one would expect, at 10 weeks, there was activation and expansion of various immune cells including CD3+CD4+ and CD3+CD8+ effector memory cells (mature cells that can be recalled to fight a pathogen), transitional B cells, and plasmablasts. At 10 months, Covid-19 patients had significantly lower total leukocyte counts, which means significantly fewer neutrophils, monocytes, and lymphocytes. Neutrophils were already lower at 10 weeks but continued to decline at 10 months. Among the lymphocytes, both Natural Killer, T and B cells were low.
Monocytes were lower at 10 months only in Groups 2 and 3. B cells decreased in all groups, but they plateaued in Group 1, yet significantly dropped in Groups 2 and 3. This means Group 1 (lower to moderate decrease in Nucleocapsid antibodies at 10 months) had a more stable immune response.
Given the extension reduction of lymphocyte number after an extended period, the authors wanted to know the effects on naive and memory T cells. RTE (Recently Thymic Emigrated cells, basically “baby T cells” newly generated in the thymus) were comparable between infected and non-infected at 10 weeks but dropped to almost half at 10 months, with CD4 cells dropping more drastically than CD8.
An increase in number of central memory CD4 and CD8 T cells was observed at 10 months, which is expected, memory cells are what enable your immune system to avoid being reinfected by the same things over, and over again.
What about B cells, the antibody-producing cells ? A similar trend, significantly lower numbers of circulating Memory B cells were observed at 10 months. A very important finding “another interesting finding was the fact that the subset of CD5+ B1-like marginal zone B cells was found to be severely reduced at 10 m in absolute”.
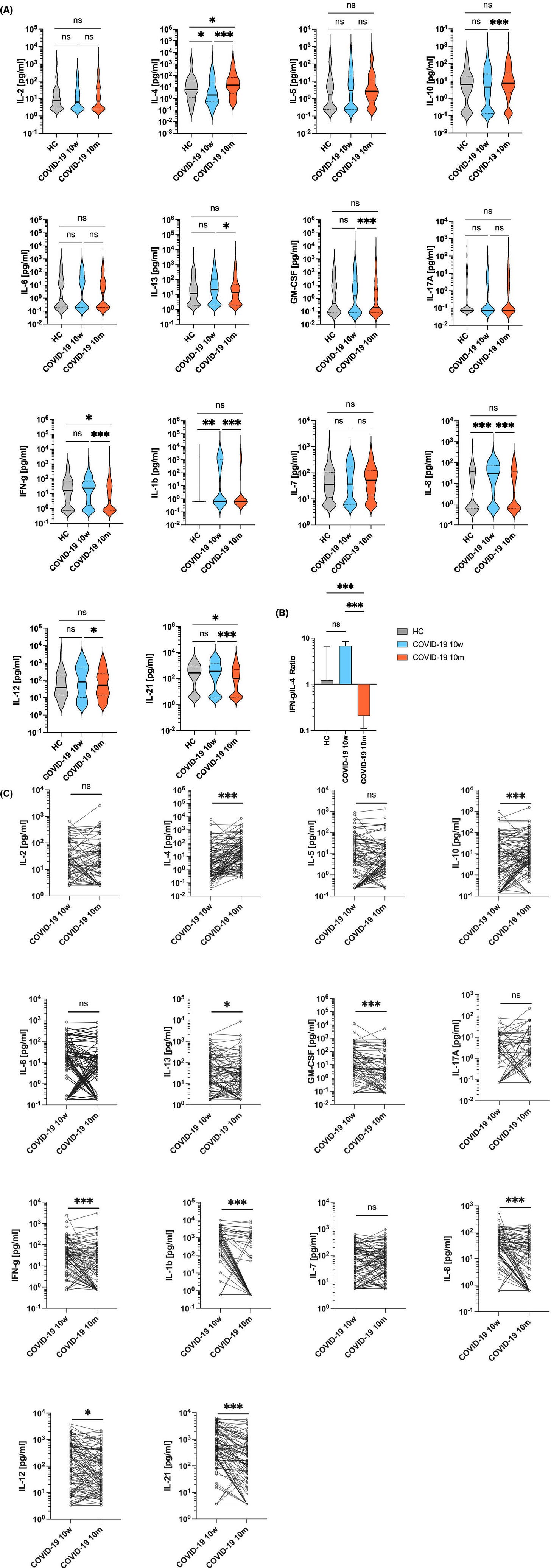
The following step was measuring systemic cytokine and if a shift between types of immunity occurred.
The cytokine profile changed significantly from a Th1-dominated response at 10 weeks to a Th2-dominated immunity at 10 months. This shift had a substantial change in the IFN-γ/IL-4 ratio, indicating a transition from a pro-inflammatory to an anti-inflammatory cytokine environment. Group 1 patients exhibited a moderate change in this ratio, whereas Groups 2 and 3 showed a more pronounced shift, reflecting a more substantial immune alteration.
So how or why would this occur ? How can a viral infection cause a significant decline in your immune cells months down the road, without an active, persistent chronic infection ? Well the authors themselves propose, citing evidence, of similar dynamics we have covered and proposed here. The first one is “simple”.
The first paper was heavily criticized by the experts, it was retracted to the bitter disagreement of the authors, but as time went on, the evidence kept mounting. And this is precisely one of the mechanisms the authors proposed. The potential infection and consequent death of Stem Cells, thus lead to an overall decline of many of the immune cells measured here.
Now “How is God’s green Earth is this monstrosity getting inside the bone marrow ?” you may ask. It is not an easy task, not usually, and needs to be done covertly. Chimerically.
I left the following paper out of the article above because I thought it belond in a special position in Part II. Well, HMGB1 is a master regulator in the bone marrow. HMGB1 is also called “Endotoxin-binding Protein HMGB1”, and as one would expect “Endotoxins induced different changes in the cells of bone marrow. Also, lipopolysaccharide caused significant decreases in red blood cells, white blood cells and platelets counts, hemoglobin content and hematocrit percent.”
The shift towards Th2 has major significance. When there is an imbalance between IL-4 and Interferon-Gamma, you can get things such as unexplained recurrent spontaneous abortion. It also plays an important role in Chronic Lymphocytic Leukemia it delays antitumor activity. Worst of all, IFN-gamma is required for viral clearance in the Central Nervous System, so we finally have a level of evidence for my argument that the virus and its pieces are persisting in the nervous system of many. Low levels do not cause significant inflammation, enough to induce systemic changes.
Marginal Zone B cells, a subset of B cells from the spleen play a critical role in the production of antibodies, and also T Cell responses to blood-borne foreign antigens. These cells play a significant role in the immune system, they bridge the innate and adaptative immune system. They also play a dual-edge role being pro and anti-inflammatory, and they are potent producers of IL-10, thus strong suppressors of inflammation. IL-10 is known to ameliorate chronic inflammation.
So why would these Marginal Zone B-like cells be depleted significantly at 10 months ? This is the second mechanism proposed by the authors. Antigen persistence, and in my opinion, Superantigen persistence (SAgs). SAgs fragments can remain individually inactive, but when interacting with cell surface antigens, and in my assessment of other proteins in the body, they become biologically active. Superantigen can create a “hole” in B-1 repertoires. Superantigens, specifically SEB will also decrease RTE, the super new thymic immune cells.
MZ B cells also play a very important role in delaying with both bacteria and its byproducts, especially endotoxin, so a significant loss of these cells over 10 months can explain the weird behavior of many bacteria diseases post-2020.
Antigen persistence will occur, and RNA persistence, both alone, and in complexes has already been categorized, but this “extra step”, superantigens will also aid in the expression HMGB1, which can quite literally induce most of the complex pathways you just read. Same for the delayed death of immune cells. Least we forget the most significant contributor and Superantigen-creating forgotten viruses.
While this article isn’t exactly long, it is complex, so I will end here, but I will refer to it in my next article, about Long Covid, because all the pieces are coming together. Because Galectin-9 plays here too.
If you choose to support my work, thank you, couldn’t do it without my supporters !









What is the distinction between vaccine and virus is the initial hit, and the middle of the road. Virus has many biological kinetics and hundreds of interactions that create all these complex pathways.
The vaccine has the mRNA translation and especially the LNP (plus some contamination serving similar purposes of the viral infection interaction with other proteins). The end of the road is similar.
If one does something, the other will do it too, at some level, per the evidence. Reminder that the T cells of unvaccinated and vaccinated now respond differently to the virus. Ain't getting simpler.
Great piece. Thank you. Things are starting to come together indeed.
My monocytes have stayed steady throughout these last 4 years. Neutrophils were down before the Jan 2020. I think bacterial infections like leprosy and TB is what I am expecting. Chronic, difficult to treat infections, and with TB needing several drugs for months, none of which are easy to take.