The long-term immunological shift in Long Covid
All roads lead to Rome
There is an announcement in the comments.
Shortly ago, two very important Long Covid papers were published, and not only do they provide a “longer term” perspective in biological markers much needed to understand SARS-CoV-2 as a whole, and provide longitudinal (over time) data, but also, we finally peer into some overlooked and important mechanisms.
To refresh your memory, since it has been quite a while since we mentioned or I shared any data or papers on this. One of the central pillars of my general hypothesis on the paradoxical nature of SARS-CoV-2 has been both the acute (short-term) and long-term shift in immunological responses in a systemic manner, and both participate and contribute to the different forms of damage we have covered.
A particular shift between your T Helper cells, which help shape immunological responses, from both a classic Th1 (inflammatory) shifting towards a Th2 (allergic) to a paradoxically pathogenic Th17. Paradoxically, because “somehow” they all end on Th17.
Too strong, acute increases in Th17 can create systemic inflammatory responses and damage specific organs, especially the gut and endothelial lining, connecting a lot of the distinct damage we have analyzed throughout the past years. A weaker response over time, you get predisposition to different infections. A persistent, chronic shift into that state, inflammation, and immunological dysfunction, potentially leading to autoimmunity, and contributing to higher chances of developing cancer and neurodegeneration.
T Cell Dynamics in COVID-19, Long COVID and Successful Recovery
To preface this study, this was done in a Russian hospital, where everyone was infected with the original Wuhan strain, which can leave the deepest scars in the immune system and in the body. 41% of the patients were vaccinated with the Russian adenoviral vaccine (Sputnik V), while some could argue that Long Covid is actually “Long Vaccine”, over half of the patients didn’t take a vaccine.
Also in line with both early and current evidence, reinfections were common among Long Covid patients. If you want to understand the complex dynamics of Long Covid, a gross yet accurate simplification is the following. One infection per year leaves your chances of developing Long Covid symptoms extremely low. Covid + other infections or worse, multiple Covid infections within a short time, you are “stacking” the chances of developing the umbrella of symptoms that define Long Covid.
An argument can be made that T-Cells have been our last line of defense against severe infections since the first strain, and that is the catch. We rely heavily on our T-Cells dealing with the virus, yet the virus deeply affects T-Cells as a whole, this being the reason the authors wanted to understand the dynamics. The patient groups in this study were people experiencing infections (acute group), convalescents (patients who recovered from Covid without problems), Long Covid, and naive, ergo never infected.
At the surface level, all groups shared similar levels between their CD4, which bridges the communication between T-Helper cells, and CD8 cells, the killer cells.
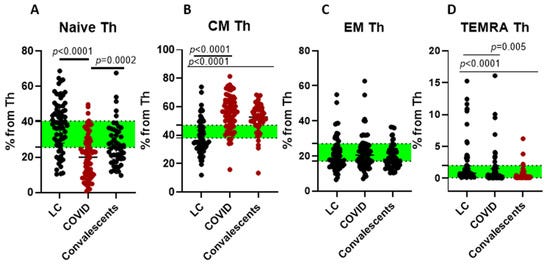
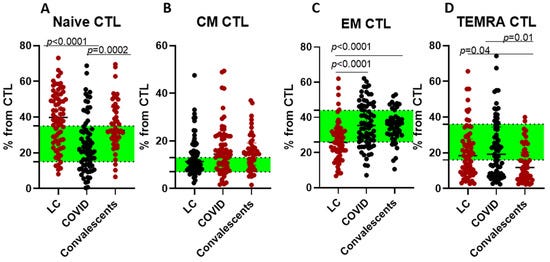
A different story is found when a deeper profiling is done. CM are Central Memory cells, that reside in the lymph nodes, basically the cells that remain at a ready-state to respond quickly when encountering the same pathogen again, EM are Effector Memory, patrolling cells in the blood and tissues. TEMRA are Terminally Differentiated Effector Cells, they don’t proliferate further but are highly cytotoxic, the “last line of a potent defense”.
T-helper subset cells in acute cases experience a significant reduction in naive (new) Th cells and an increase in Central Memory cells compared to healthy people. Convalescent individuals were evaluated 1 to 3 months post-infection have, unexpectedly, similar Th cell profiles as acute cases. This points to an incomplete recovery, which is in line with evidence. It takes 4 months, minimum, for the immune system to recover from the damage Covid induces in lymphocytes.
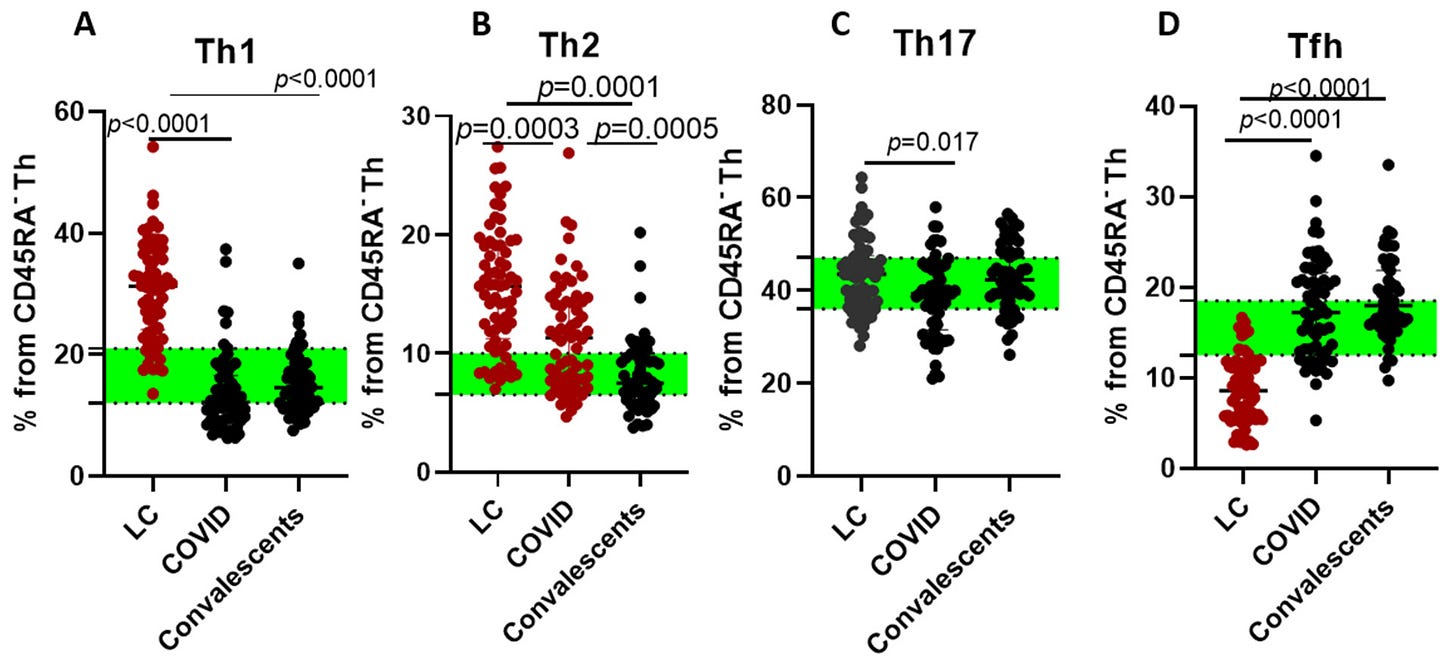
Here is where we verge into the paradoxical nature of SARS-CoV-2. Measuring the subset of T-Helper cells, the authors found a strong polarization in Long Covid patients towards Th1, but also Th2, which is paradoxical. Either you are on Th1 (inflammatory, used to fight viruses, etc) or Th2 (allergic, against parasites), and this is something I brought up back in 2021, that there would be a long-term shift towards Th2, while Th1 remained elevated, ending up in Th17 pathology in a number of infected people.
You can also observe a somewhat high level of Th2 in patients infected with Covid. Unlike all groups, Long Covid patients have much lower levels of T-Follicular cells, necessary for high-quality antibody production, low levels indicate a poor antibody response against the pathogen.
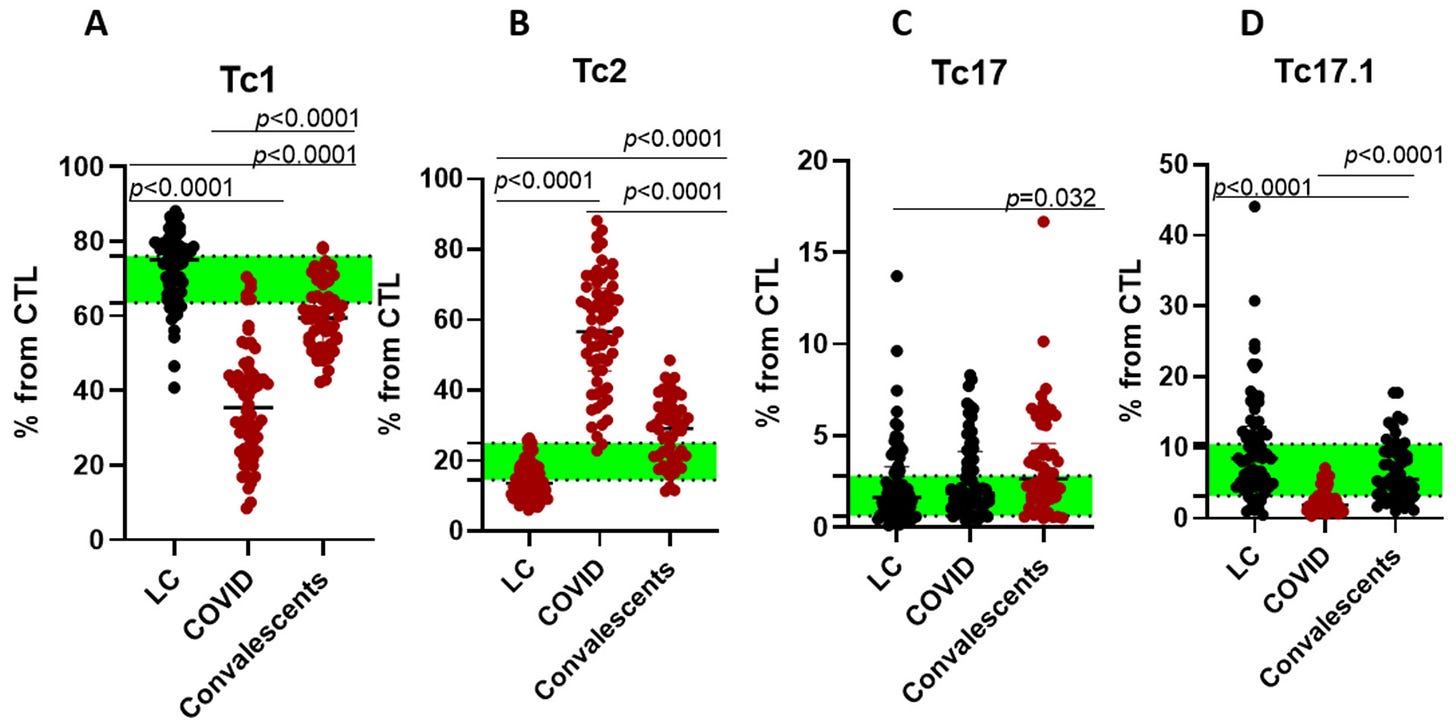
This trend is also observed in cytotoxic, CD8 cells, where Tc1 (similar to Th1) have lower levels in acute infection, and higher Tc2, this is a shift from normal antiviral responses, suggesting immune dysregulation, and again, even Effect memory (EM) cells showed the same shift.
While Long Covid patients attempt to increase the production of new T-Cells (naive), TEMRA, the end-stage for highly competent T-Cells have lower levels, the body is tries but fails to differentiate these new cells into the more functional subsytes, this can be seen in the EM2, 3, and 4 in the image above.
So what is happening here ? The short answer is that there are persistent, low-grade inflammatory signals coming from different sources in Long Covid patients, shared by infected patients, but at a point in the infection, Long Covid patients fail to stop these signals and recover. This persistent inflammation draws immune cells to tissue, which can’t be cleared properly, causing Long Covid symptoms, even if other measurements and biomarkers are normal.
This is somewhat confirmed by the Th2 and Th17 long-term bias, the body is reacting against itself as it can’t clean viral remnants and tackle persistent signaling. Allied with deficient T Follicular cell production, it tilts the body into poor antibody responses, poor regulation of immune responses, and can “tilt” the body into autoimmunity. Even the new (naive) T cells produced in the thymus are skewed towards inflammation.
This shift both occurs long-term and lasts when the immunological dysfunction persists. Before any attempt at writing on the further implications of this, we need to cover another Long Covid paper, this time in children.
Immune-Metabolic Programs Drive Disease Trajectories in Paediatric Long COVID
Contrary to popular belief and exemplified by recent papers, Long Covid is not “rare” in children, or adults for that matter, and yes, vaccination swings this both ways (protective/harmful for Long Covid alone, not referring to any other detrimental effects). It is increasing at a significant rate, and knowing exactly which pathways it hits, if there are any similarities with their adult counterparts, can help mitigate and treat it. A large portion of the children in this study were infected with Omicron, and it was conducted in Germany.
This research takes a more comprehensive look into pediatric LC, not focusing solely on the immune variables, but also metabolic. The breakdown of patients in this study are 74 children and adolescents with LC throughout up to 3 years post-infection, and 2 control groups, 14 healthy children, and 13 children with Cystic Fibrosis under control, these patients serve as a baseline so you can separate what is specific to Long Covid, and what is “merely” a byproduct of repeated infection or chronic inflammation.
Within the first year
Interestingly enough, both IL-6 and TNF-Alpha, both strong pro-inflammatory proteins and markers, were at the same levels in both healthy children and children with controlled Cystic Fibrosis, thus they were considered a single control group. Following LC children over a year and measuring IFNα, a central cytokine for immune response, showed it remained elevated, but the complement system participants C3, C4, and CH50 remained in the normal range, these are part of the clotting system, and this is the opposite of what you see in adults.
Regardless of age, LC patients will often experience severe fatigue and shortness of breath, thus, lung and heart involvement are always tested, and here there was no cardiac involvement. Using K Clustering algorithm, which analyzes the data and creates clusters of patients based on their shared markers or similarities, they found 3 subgroups of LC children with distinct lung function between them.
Without IL-6 involvement, the authors deduce that there must be other very important proteins that influence lung inflammation, choosing IL-13 and IL-33, both highly significant in that regard, but it goes beyond it, both of these proteins are directly related to Th2 immune responses, the allergic ones, and IL-33 is directly responsible for Th17 responses, IL-33 is also a pillar in mucosal immunity, and it is invovled in tissue repair, so it can do both, inflammation and healing, and both remained elevated.
A more detailed breakdown of the systemic immune response in the LC children found that Th2-related cytokines (IL-4, IL-5, IL-10, and IL-9) were the same as controls, but Th1-like, those being Th17 and 22-like cells, found a skewed Th2/Th1 ratio, among the Th17/22, IL12p40 (a small part of IL-12, biologically active) was significanty higher, and so were IL-1α and IL-1β, these 3 can shift the immune system into a Th17-centric response.
Similar to the first paper, there is a “coexistence” of paradoxical immune responses in Long Covid, even in children. Given the complex immune interactions, and how autoantibodies (meaning your antibodies attack your own cells) and other organs, especially the brain and nervous system are involved in LC, this was their next step.
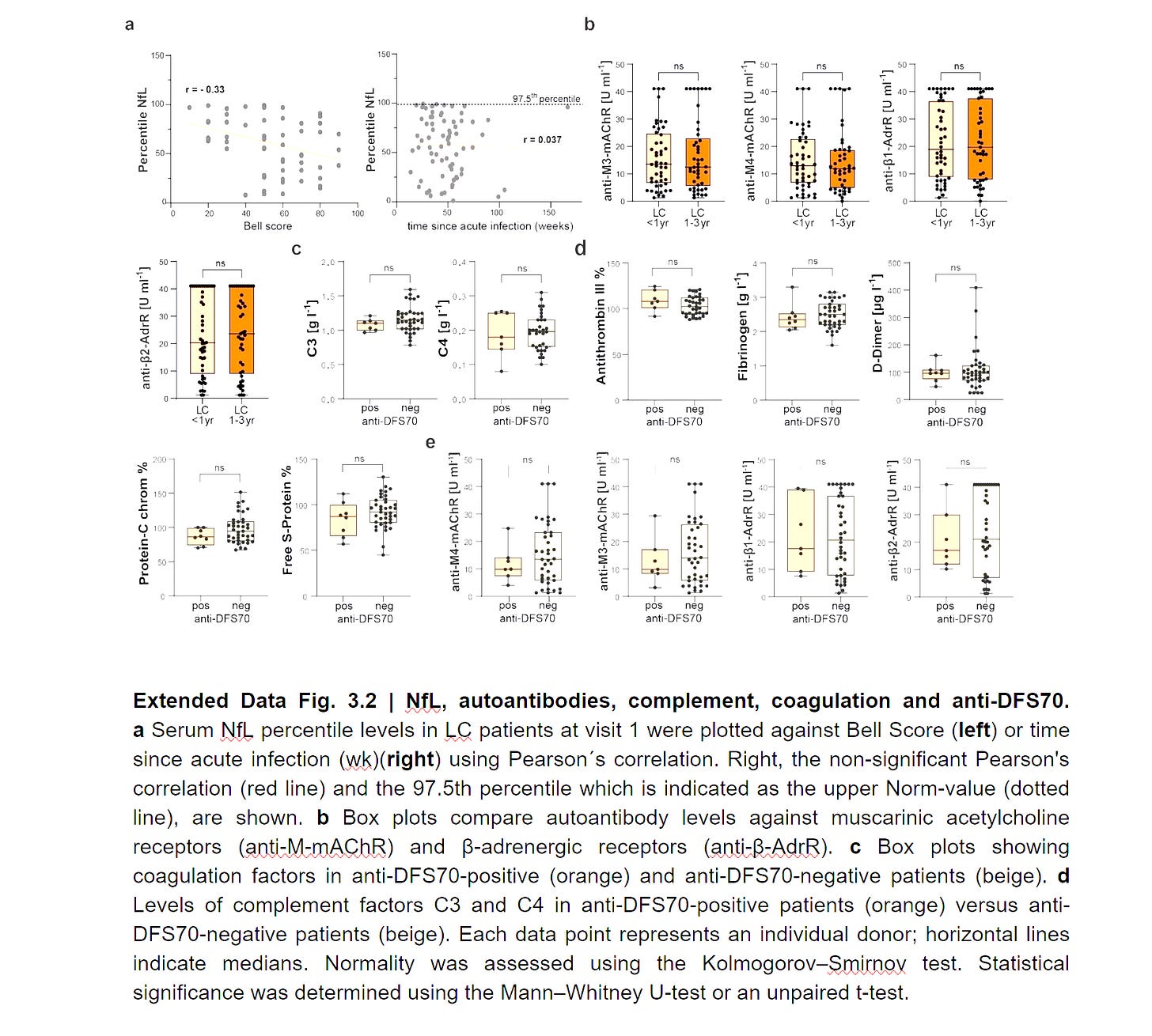
Per the A. graph, using NfL (a biomarker for neurological inflammation and injury, especially ongoing injury), and the more neurological debilitation there is, the higher their NfL is. And in some children, it doesn’t matter how long their infection was, NfL remains elevated, thus there is ongoing, lasting neuroinflammation.
On the autoantibodies, well, grace was to be found as there wasn’t really no significant increase in autoantibodies, somewhat contrasting their adult counterparts. I also like to bring to your attention that the authors measured β1- and β2-adrenergic as well as M3- and M4-muscarinic acetylcholine receptors, and didn’t find anything. What I want to bring to your attention, in my experience over the years, autoantibodies to these receptors are 95% of the time, only present with Coxsackievirus, a known latent pathogen.
Next, they measured anti-DSF70 antibodies, usually positive markers, people with these antibodies have lower chances of developing systemic autoimmune diseases, but here is for the distinction of subgroups. No children in the control group tested positive, but 11% in the LC group did, and the ones who had the antibodies had them even after months. Intriguingly, children positive for Epstein-Barr Virus didn’t test positive for DSF70.
Beyond the First Year
After the first year, the systemic immune responses were measured again, this time, the antiviral response, measured by IFN-α, declined. The Th2-skewed state (Fig. 3b, Extended Data Fig. 3.1a) revealed a marked reduction in IL-4, IL-13, and the type 2-alarmin IL-33, accompanied by a two-fold rise of IL-9, pointing towards a shift towards a Th9-like state. Within the Th17 immune axis, IL-23 and IL-12p40 increased, while Th1 remained the same. This means over the long term, LC in children is skewed towards a Th9/Th17 type, which is both immunosuppressive and inflammatory.
Prior exposure to EBV has a drastic impact on the subtype of LC a child can develop, per a couple dozen of my articles over the years. Children with prior exposure to EBV, thus testing positive for its antibodies, had a significantly more inflammatory and more autoimmune-like response, with significantly higher levels of IL-1α, IL-15, Th17/22 cytokines (IL-12p40, IL-22), and neutrophils. They also had autoantibodies against prothrombin, indicating a coagulation shift.
In children without exposure to EBV, they had a distinct form of Long Covid, which was not correlated with a similar inflammatory response, but it was mostly a metabolic and haematological dysfunction, with low thiamine and low Mean Corposcular Hemoglobin Concentration (MCHC) correlated with a more severe dysfunctional state.
Low Thiamine affects a lot of what is covered here, especially a shift towards Th17, but also it shows mitochondrial dysfunction, and low MCHC indicates impaired red blood cell function, improperly carrying oxygen. Interestingly, in this group, higher levels of IL-12p40 were found to be regulatory, protective.
The Neopolymorphic complexity of SARS-CoV-2
(I am referring to this article of mine)
In late 2021, I shared this paper, which covers specifically the role of Th17 cells in viral persistence and inhibition of T-cell cytotoxicity. How does this work is by a flood of inflammation, often mediated by IL-6, and as we covered here and elsewhere, this enables a shift towards Th17, and these cells will enable the persistence of viral fragments and pathogens themselves, creating a feedback loop of persistent presence of Th17 cells, driving chronic inflammation. EBV by itself can prime the body towards this response, too. My second reference.
The paper above, as with quite a number of other papers I analyzed throughout the last 18 months, uses non-vaccinated data, and another point is no reinfections, it is purely the effects of one (nasty) strain. Even though the paper covered above does not directly measure the cytokines involved in Th17 (and Th17 is tricky to measure, given it is the latest cell to develop in tests), there is a drastic decline in IFN-γ and a long-term shift towards Th17. IFN-γ is a natural inhibitor of Th17 cell development.
Allied to another long-term decline in Regulatory T-Cells, it aligns with the findings of the papers here and other papers I covered. Over the span of many months, there is a shift towards a Th2 response, and for a short time, a Th17. Most people, even patients who develop Long Covid will often recover from both and reach equilibrium.
The concern is that literally almost everyone infected shares similar pathways and a similar end of the road. Even the reduced thymic output is observed in a mild Omicron infection, and it lasts months. A loss of immune cells over almost a year has drastic implications when you suffer from almost a yearly infection.
Ending notes
Throughout this year, a few people messaged me asking about their persistent cognitive symptoms after a mild Covid infection, these are all unvaccinated, and they all shared similar symptoms. “Slow thinking”, distinct from brain fog, mild forgetfulness, and sometimes the inability to deal with complex issues, they all recovered quickly with the same suggestion.
High dose thiamine (500 mg). Many of my long-standing suggestions work, but the differential this year was Thiamine, most people don’t supplement B Vitamins, let alone Thiamine by itself. Thiamine is one of the only vitamins I consistently, since 2020, recommend daily, long-term usage. It is also why I am experimenting with high-dose creatine and why creatine works so well for Long Covid, because it directly addresses the bioenergetic fallout. I don’t have Long Covid, I just wanted to see what 20 grams of creatine per day would do to me.
Avoiding the systemic inflammatory response present in any infection, feeding the body with the proper nutrients for both limiting the infection and aiding a quicker recovery, enables the body to deal with the viral fragments, which occur in anyone. The better your immunological health, the smaller the likelihood of having a significant amount of viral fragments, thus overburdening the body.
Paradoxically yet again, these pathways are what enable the persistence of fragments in the body, creating not one, but multiple feedback loops. My suggestions remain the same (in the series of articles called Heal Thyself). If by any chance you find yourself struggling to recover, even with supplementation, your recourse is peptides, which will, 99% of the time, enable the body to tackle anything and move the recovery needle.
Consider becoming a paid subscriber, it helps support my work ! And if you are, thank you !




As I shared shortly ago on Twitter. My laptop completely died. When the GPU started failing, it was already marching towards its inevitable end, I am surprised it was quicker than I expected.
I still can work/write using my tablet, but the workflow is completely different and takes more time. I will either focus on more essay-ish articles or just take longer to write, which bothers me.
This will last a few weeks until I figure out things (a new computer). Your support and patience are appreciated.
The next article will inevitably be the sequel to Language The Genocidal Organ.
I wish you all a great week ahead.
I loathe acronyms.
Had I paid better attention in immunology lectures I still would not be able to read this essay as they didn't even describe CD4+ and CD8+ cells in clinical use until the AIDS epidemic flared in the 1980's.
The first graph presented does not define CD3 or even more obscurely CTL.
When I snivelled about my acronymophobia to one of our consulting psychiatrists in 1995 his sympathetic reply was brief: "Oh no! Not AP!"
Computer problems are a nuisance. My ten-year old I7 desktop and laptop are planning simultaneous failures while I am having a cash-flow crunch. Maybe with new tariff nonsense you will be able to find a deal in something that wasn't shipped to the US.
Best meme of the week was a panel of President Trump: "My government isn't working for me." Next panel: "Have you tried tuning it off and then on again?"