This article cuts “closer to home” than others, mostly the first paper, and understanding this context is needed. Long-time readers will be aware that I have suffered from stomach issues for many, many years, but I experienced significant improvement in the last 2 and a half years, so I have a particular interest in gut issues.
The context part comes now. For years, I stated I could tell I was infected with SARS-CoV-2 by how my throat behaved, it felt inflamed at first during the infection, but post-infection, it felt as if it had been eaten away. The second is how my father died, a very painful and slow-to-crawl death from “throat cancer,” thus an inherent fear of having the same.
As usual, thanks to my reader Dee for getting me this paper =). I will preface the entire article with a brief and how you can address what I am about to cover.
The viral infection affects the barrier protecting your gut and throat from further damage and inflammation, leading to more inflammation, dysfunction, and immunological shifts that can contribute to lasting symptoms and Long Covid. How can you address it ?
One of the best supplements for gut recovery is Glutamine, it calms the gut, it fuels your immune cells to fight pathogens, and it especially helps your gut to heal. Creatine will help to speed this process rather than acting by itself. Taurine will also help, sometimes it makes a substantial difference. Melatonin, and 5-HTP too, this last one mostly if you have serotonin problems.
A break glass in case of emergency, meaning a more expensive but faster recovery route is peptides. BPC-157 + TB500, injected into your belly fat. Thymalin if you have significant immunological dysfunction. There are many, many other supplements that you can address these problems, but these are the ones I have had more success with over the years, on myself, and hundreds of people I have directly helped.
Impairment of Esophageal Barrier Integrity: New Insights into Esophageal Symptoms in Post-COVID-19
Gastrointestinal symptoms are common both during a SARS-CoV-2 infection, with lasting dysfunction being present in many of the severe and long-lasting (Long Covid) cases, especially being the case in the post-Omicron era, given that Omicron didn’t cause pneumonia, and the most observable symptom was the gastrointestinal ones.
Even recently, articles I have written have discussed how important gut health is, especially the gut barrier, and maintaining integrity, dysfunction, or permeable barrier (leaky gut) leads to poor absorption of nutrients, further dysbiosis (more bad microbes, fewer good ones), potentially fueling long-term chronic diseases. Some of the more pertinent articles.
A total of 55 patients participated in this study, with almost 62% being male and the average age being 46. 36.6% were hypertensive, 25.4% diabetic, and 25.4% obese. The most common symptoms during hospitalization were dyspnea at 60%, diarrhea in 34.5%, and nausea or vomiting in 27.3%. During hospitalization, and this part is very important, 41 patients (74.5%) required oxygen therapy, 49 (89.3%) received antibiotics, 47 (85.5%) corticosteroids, and 32 (58.2%) were prescribed anticoagulants, only 2 patients used Proton Pump Inhibitors, most commonly prescribed drug for acid reflux, gastritis and gastrointestinal conditions.
The researchers did upper digestive endoscopy and biopsies, something you don’t see in many papers but it is becoming a good new trend, 25 of the 55, and the control group never had infection with SARS-CoV-2 or with gastroduodenal symptoms consistent of 8 patients.
Heartburn and acid reflux, some of the most common symptoms of gastric diseases, significantly increase in post-COVID patients 3 to 6 months after discharge compared to what they experienced during hospitalization. Next, they tested how permeable the esophagus was by using a test called TEER (Transepithelial Electrical Resistance), which measures the electrical resistance across the tissue. Higher resistance = tighter barrier = better.
TEER between Covid patients and controls was basically comparable, similar, no major differences, but using the fluorescein test, which measures how easily small molecules pass between cells, showed something different. This test found significantly higher permeability between post-COVID patients compared to the control, particularly when the tissue sample was exposed to acidic conditions. Covid made the esophagus much “leakier” especially when exposed to acid (which… SARS-CoV-2 will itself induce).
They also measured and found elevated levels of IL-8, an inflammatory cytokine that acts to attract immune cells to a location. IL-8 has been implicated in severe cases and in lasting damage since 2021, and here they found it in higher levels in the biopsies, even after months, the infection cleared. If you recall one of my recent SARS-CoV-2 articles, the virus attacks and damages the cell’s ability to clean mucus effectively, thus allowing inflammation to persist for longer.
They also found increased expression of Claudin-2, a protein that forms pores in the paracellular space, thus, it quite literally makes the barrier around your throat leakier, and both Claudin-2 and IL-8 will make your throat more susceptible to damage from the gastric acid. This creates an inflammatory loop (weakened barrier → acid penetration → inflammation → more barrier damage, repeat weakened barrier step →).
Other inflammatory proteins that are often found increased in other areas of the body and tests, with IL-1ß, IL-6, and TNFα being the posterchild, were not increased. So, specific tissue in the body may have distinct inflammatory signals. Before addressing the second paper, I need to bring an older article to your attention, and I would argue and have argued for years, the most pertinent and yet overlooked aspects of SARS-CoV-2, including its mRNA vaccines.
One of my long-running arguments has been that Endotoxin plays a central role at every single stage of SARS-CoV-2 damage, sequelae, no matter how “drastic”, but especially significant in how lasting. The mRNA vaccines themselves make use of the Endotoxic interaction for an efficient immune response at first, with lasting (epigenetic reprogramming) effects, and so does the virus, endotoxin is what allows the virus to deliver its payload at locations that shouldn’t have virus.
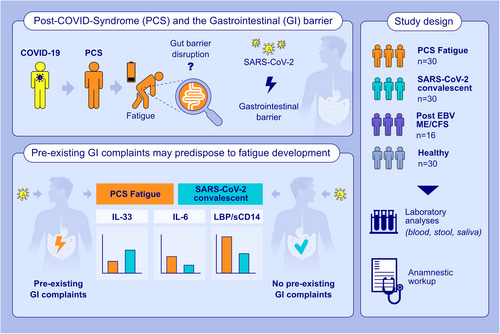
Gastrointestinal Barrier Disruption in Post-COVID Syndrome Fatigue Patients
PCS is one of the terms used for Long Covid, and this is largely a vaccinated group of patients. Given my experience and years of research on SARS-CoV-2 alone, this doesn’t make the study worthless, as many may jump to the conclusion, but it does paint a rather darker picture for the mRNA vaccines. Not that this is a hard thing to do.
It is no secret that pre-existing gastrointestinal conditions make you susceptible to further disruptions, and half of the Long Covid patients had it before, also interesting to note the “frequent events of sickness and infections” in 40% of the PCS patients, and a whopping 87.5% of the ME/CFS. PCS patients often had cardiovascular symptoms together. The vast majority of patients here, unlike the other study and many others, had asymptomatic or mild infection.
To remind you, a vaccinated person responds to the Spike Protein from the virus in a distinct manner. We (unvaccinated) and the vaccinated target different regions of the Spike Protein, while how each group responds to the Spike Protein has yet to be taken into consideration, and a method to properly assess this needs to be developed. I foresee this as an important measurement in the future.
No SARS-CoV-2 was detected in the blood, stool, or saliva samples, and here the authors decided to use the Envelope Protein, which is a better marker for active replication, because both Spike and Nucleocapsid can persist for longer periods, giving false negatives of lasting live virus.
A Leaky problem
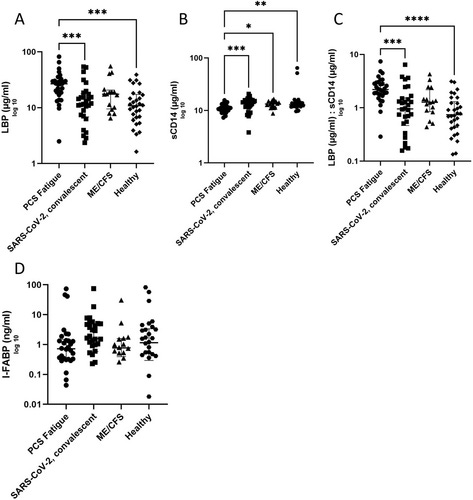
One way to measure Intestinal Barrier function, or leakage, is by measuring LBP, Lipopolysaccharide Binding Protein, a protein that binds directly to Endotoxin, starting and enhancing your immune response towards bacterial toxins, and depending on many variables, removing the toxins.
sCD14 is a needed co-factor together with LBP to mediate your response against LPS, and measuring the ratio (how much of each) between LBP/sCD14 can indicate leaky gut. LBP was found to be at higher levels in PCS than in other groups, and PCS had lower levels of sCD14. This effectively means there is endotoxin passing through the gut to the bloodstream, and an immune dysregulation making it harder for the body to deal with said toxin, contributing to a persistent, low-grade inflammation.
You can measure the intestinal barrier integrity by using specific markers, rather than other more invasive tests, and as such, the authors used such markers, these being IFN-γ, TNF-α, IL-6, IL-1-β, IL-8, and IL-33. A significant elevation of IL-6 with a reduction of TNF-α and IL-1-β was observed in PCS patients. IL-33 was oddly significantly decreased in PCS patients, compared to SARS-CoV-2 negative controls, IL-8 and IFN-γ levels did not show statistical significance nor a disease-specific pattern. Which I attribute to Long Covid type and the time of testing.
Significantly low levels of IL-33 are rather intriguing because one of its functions is the maintenance of the gut’s epithelial barrier, protecting it, and overall gut health. Low levels indicate a failure in the protective immune response, compromising the barrier integrity, thus contributing to low-grade inflammation.
Stool sample analysis of pro-inflammatory markers found no relevant alterations, such as Calprotectin used to measure gut inflammation, Beta-Defensin-2, an antimicrobial peptide in the gut, zonulin peptides, proteins that modulate permeability, and serotonin, a neurotransmitter of the highest importance in the gut, and gut-brain axis.
I would very much prefer the measure of all these markers to be at least in the blood, especially serotonin, which gives the importance and how dysfunctional this neurotransmitter is at multiple times in Long Covid cases and types. Also intriguing is the fact that they found no significant difference in the fecal microbiome in these patients, but again, I would prefer other forms of measurements, still valid.
In this particular patient group of Long Covid, the body is attempting very hard to adapt to the constant exposure to low levels of Endotoxin, while mitigating inflammation, leading to a chronic inflammatory state, which contributes to the cardiovascular symptoms, but especially the fatigue. It also triggers a dysfunctional immune response in and outside the gut. Pre-existing vulnerabilities or a subclinical but significant response towards the mRNA Spike Protein intensify the problem.
The data by itself (while completely consciously excluding the mRNA vaccination effects) already points towards a state of immune reprogramming induced by chronic low levels of endotoxin. Compensatory mechanisms in response to high levels of IL-6 will lead to low levels of other inflammatory mediators, such as TNFα/IL-1,β, in some cases. It indicates a non-canonical state of Endotoxic Tolerance if you will.
The next article is as important as every other article I have referenced here and previously. Because the findings are very pertinent.
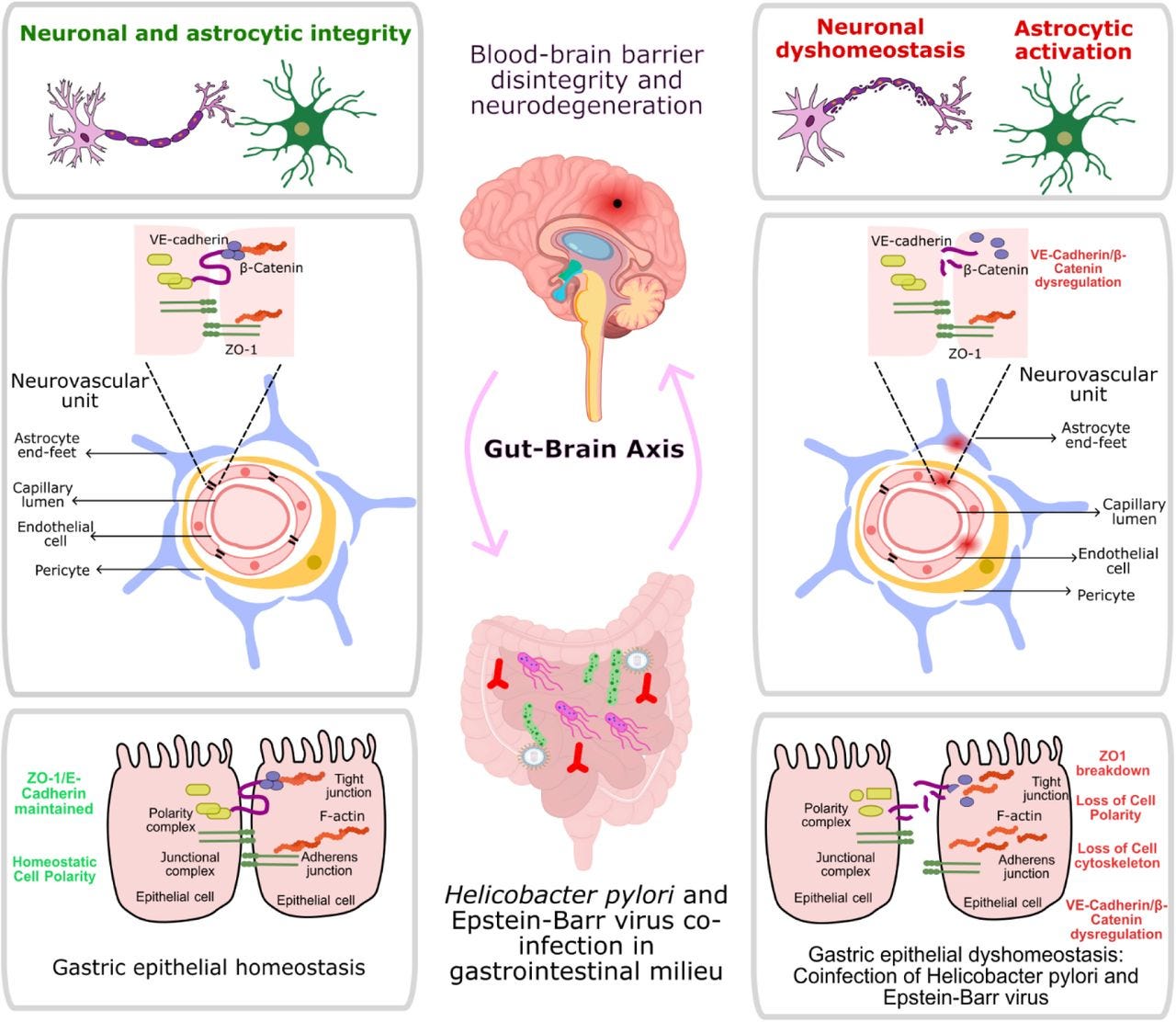
Epstein-Barr virus and Helicobacter pylori Coinfection Drives Gut and Brain Barrier Dysfunction
Biological barriers, including blood-brain barrier (BBB) and gut epithelial barrier, are essential to maintain homeostasis and provide protection against pathogenic stress. Here, we investigated the impact of Helicobacter pylori-Epstein Barr Virus coinfection on gut-brain axis integrity. Our results demonstrate that coinfection induces significant disruptions in tight and adherens junction (TJ and AJ respectively) proteins in gastric epithelial cells, including downregulation of ZO-1 and E-cadherin. The secretome from these coinfected cells significantly compromises the integrity of BBB-derived endothelial cells, including cleavage of VE-cadherin, loss of TJ proteins such as Claudin-5, and enhanced permeability.
Furthermore, the sole exposure of mice to coinfected secretome lead to the loss of cerebral VE-cadherin and ZO-1 and the induction of neuroinflammation, characterized by elevated pro-inflammatory cytokines, TNF-α, amyloidogenic accumulation, and neurocognitive deficits. The secretome driving such forces potentially carries pathogenic metabolites, host inflammatory cytokines and metabolites that might contribute to disease pathogenesis as observed in this study. Together, our current study provides novel insights into how coinfections contribute to gut-brain axis dysregulation and neurological pathogenesis.
SARS-CoV-2 and its Spike Protein by itself will cause a lot of your “barriers” to weaken and become leaker, especially and more perceptible at large your gut barriers, but as I have brought up since 2020, the real problem has always been its close friendship with, quite literally, every other pathogen known to man.
Viral reactivation is now recognized as one of the hallmarks of SARS-CoV-2 and even Spike exposure, but an overlooked by the public aspect is SARS-CoV-2 co-infection or post-infection with H. Pylori.
Here, the authors found a novel pathway by which co-infection with H. pylori and EBV leads to a complex interaction that compromises the gut barrier by affecting the tight junctions of the epithelial cells, not in a dissimilar manner to SARS-CoV-2. This leads to a leaky gut, and the content of these cells will inevitably reach the brain, and this will induce a leaky BBB. Pathogenic debris in the brain is a hallmark for the accumulation of misfolded protein, such as amyloids, which are naturally antimicrobial at first.
Also, from my personal experience of almost 2 decades, gut issues take years to show observable and measurable symptoms, and in many people, they simply don’t until they have a nasty ulcer and are put on strong medications and the most bland, soul-killing diet known to man.
Within my theme this past year, it is why I bring these to attention, as each infection contributes mildly to the effects described here, the immunological and physiological respective of “slow at first, then all at once”. Taking care of your health now pays dividends later.
If you are a supporter, thank you. If you are not, consider becoming one !











Have a great weekend. For the first time in months, I feel in my gut a calm before the storm.
Anyway, if you have something you would like me to cover at some point in the near future (I have so much to write about still), let me know.
There is some research about lactobacillus reuteri helping overcome h.pylori - from wikipedia: Limosilactobacillus reuteri has the potential to suppress H. Pylori infection and may lead to an improvement of H. Pylori-associated gastrointestinal symptoms,[49] reducing specific symptoms such as diarrhea and frequent abdominal distention.[50] In the future, L. reuteri can become a central part of a strategy to avoid using antibiotics and fighting antibiotic resistance in H. pylori infections[51] and besides fighting antibiotics resistance, L. reuteri may be a great alternative treatment for H. pylori causing fewer side effects than antibiotics.