Long-term Microvascular Complications After "mild"Covid
Fibers and Creatine to help =)
I have been working on multiple articles at the same time, but also kinda enjoying my weekends (up until March this year, it was 24/7 non-stop, slowly trying to have a schedule like a normal person… although I work in bursts of hyperactivity too). But what consumed my last 3 days was organizing my tabs and taking the necessary notes on pen and paper, I had a few tabs to go through. Just a few.
Yet, the stars still align lately, to my surprise, right after publishing the Kidney-Microclotting article, I found the following article.
Post-acute COVID-19 syndrome: prevalence of peripheral microvascular endothelial dysfunction and associations with NT-proBNP dynamics
One of my focuses, and an underlying overlooked injury mechanism that can cause long-term dysfunction in many people after a SARS-CoV-2 has been micro clots (fancy jargon micro thrombi). In regards to Long Covid (PASC) it adds to the complication because it is multi-layered, systemic, immunologically complex, there are multiple sub-groups of Long Covid patients. And often Long Covid sequelae are relegated to Acute or Severe infections, both requiring hospitalization.
This paper sets itself apart from many others precisely because all patients here had mild infections, did not require hospitalization, and before vaccines were available, so “it is just the vaccine bros” will be severely disappointed to resort to Girard’s scapegoat mechanism.
Here the authors used two tests, one called Peripheral Arterial Tonometry, which measures how well the blood vessels expand and contract, this measurement is called Reactive Hperremia Index (RHI), an RHI score of less than 1.67 indicates microvascular dysfunction, above 2.0 is considered normal.
The second measures a peptide called NT-proBNP, which is commonly used as a marker for heart stress, failure, and other major cardiac events. Higher NT-proBNP means the heart is working harder than normal, and the cause could be higher blood pressure, damage to the heart itself, or… endothelial dysfunction. This was collected 10 months after the initial infection and 24 months after that collection (2 years later).
The results showed that 41% of the patients in the study had microvascular dysfunction, and another 20% had mildly impaired vascular dysfunction, meaning over half of the patients here had damage to their small blood vessels. Patients with microvascular dysfunction also had higher NT-proBNP that trended upwards over time, meaning the microvascular system is not functioning properly and it is stressing the endothelium and the circulatory system, thus the heart.
NT-proBNP levels remained below the common threshold for diagnosing heart failure, which is something I completely disagree with “science” that markers are only important in that single snapshot in time, and only at drastically different levels than the average. Even though below, the patients with endothelial dysfunction experienced an increase of 21% in their NT-proBNP levels, suggesting ongoing low-grande inflammation. There was also a significant correlation between NT-proBNP levels and the RHI.
Patients with great NT were more likely to have lower RHI, thus showing declining microvascular health. The most important aspect of this study is the long-term follow-up with patients, showing using different markers not only the presence but ongoing dysfunction and potential damage of the microvascular system, even after “mild infection”. Why is this so important ?
Besides my own “linguistic convergence” analytical framework, the scientific trends in the past 9 or so months are clear. More and more evidence of microvascular complications, long-term months after clearing an infection, and microstructural alterations. Unlike significant damage, the ones you can pick up in common blood tests, “micro” anything to the body is the medical definition of Death by a 1000 cuts.
It takes 15 to 20+ years for a compromised microvasculature to be clinically significant, clinically measurably in neurological conditions, quite literally most neurologists and vascular/circulatory system specialists will pick up only after initial symptoms present themselves.
As much as I would love to attribute these effects to a single pathway, a single “mutation”, single anything, the fact remains it is multifaceted, multifactorial, and highly complex but, there is an often overlooked, metabolic player in this thrombotic chaos. Our old friend.
A satisfactory “AI-podcast summarization” of the article.
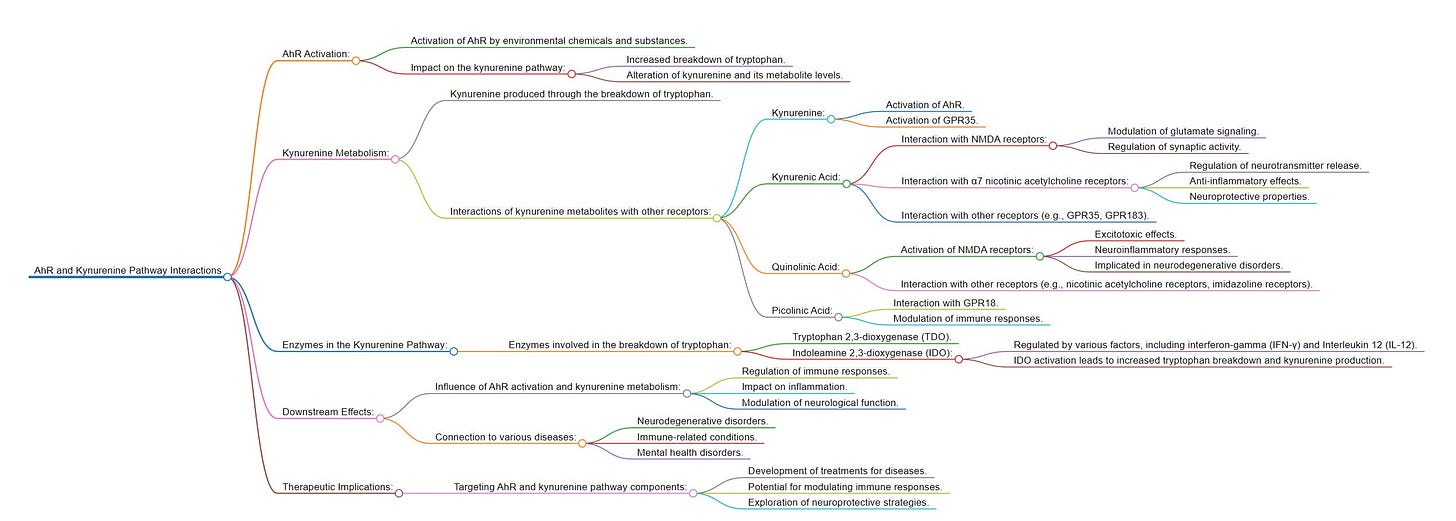
Another satisfactory “AI-podcast summarization” of the article mentioned, and a graph covering the complexity of everything mentioned within the article.
The Kynurenine Pathway always had a significant, impactful, and clearly lasting effect in all manners of a SARS-CoV-2 infection, it literally has an effect or touches a couple hundred of the articles I have written, I favor building both my hypothesis, the knowledge base, and possessing a deeper understanding. Not only people can help themselves, but so when I suggest you do X for years, I can point towards something.
Whenever you read about the Kynurenine pathway, you will inevitably see or read about the Aryl Hydrocarbon Receptor (AhR), which the Kynurenine Pathway directly modulates, and so does a myriad of other things. Clots activate the “immune cells” in your brain via the AhR. Kynurenine is a player in thrombosis, in the kidney, and heart. I am not only mentioning the Kynurenine Pathway because of these important effects, but because, years ago I stated:
“You should add natural fibers, whichever you prefer, I personally used wheat bran, for 3 purposes.
To scrap any potential virus or remnants from your gut, thus avoiding persistence and weeks of dysfunction
Aid in the recovery of systemic metabolism, avoiding glucose spikes
Modulation of your microbiome into a healthier state, and avoiding or fixing the Kynurenine Pathway
Dietary fibre directs microbial tryptophan metabolism via metabolic interactions in the gut microbiota
Tryptophan is catabolized by gut microorganisms resulting in a wide range of metabolites implicated in both beneficial and adverse host effects. How gut microbial tryptophan metabolism is directed towards indole, associated with chronic kidney disease, or towards protective indolelactic acid (ILA) and indolepropionic acid (IPA) is unclear. Here we used in vitro culturing and animal experiments to assess gut microbial competition for tryptophan and the resulting metabolites in a controlled three-species defined community and in complex undefined human faecal communities. The generation of specific tryptophan-derived metabolites was not predominantly determined by the abundance of tryptophan-metabolizing bacteria, but rather by substrate-dependent regulation of specific metabolic pathways. Indole-producing Escherichia coli and ILA- and IPA-producing Clostridium sporogenes competed for tryptophan within the three-species community in vitro and in vivo. Importantly, fibre-degrading Bacteroides thetaiotaomicron affected this competition by cross-feeding monosaccharides to E. coli. This inhibited indole production through catabolite repression, thus making more tryptophan available to C. sporogenes, resulting in increased ILA and IPA production. The fibre-dependent reduction in indole was confirmed using human faecal cultures and faecal-microbiota-transplanted gnotobiotic mice. Our findings explain why consumption of fermentable fibres suppresses indole production but promotes the generation of other tryptophan metabolites associated with health benefits.
Our findings provide a rationale for directing gut microbial tryptophan metabolism away from indole production and towards the generation of beneficial Stickland fermentation products including ILA1,2,3, IAcrA1,4 and IPA9,10,13,55 through dietary fibre interventions with high fibre and/or tryptophan supplementation
Add fermentable fibers not only suppresses the creation of indole production (the bad side of kynurenine), but aids the gut bacteria in producing the good tryptophan metabolites, the good side of kynurenines, that can provide health benefits, after all, the Kynurenine Pathway is the poster child of “dual-edge pathway” in the body. There are many other benefits to adding these fibers too, but in the context of SARS-CoV-2 effects, these are the most impactful long-term, given the contribution of the KP towards… well, everything.
And in the line of suggestions from years ago, late in 2020 and again in 2021 I advised anyone, vaccinated, or not, but especially with Type 1 or Type 2 diabetes to add Creatine. Later I wrote an article on improving Long Covid symptoms after months of creatine supplementation, among other effects, such as improving cardiovascular health, bioenergy, mitochondrial and immune function.
Eight-Week Creatine-Glucose Supplementation Alleviates Clinical Features of Long COVID
Preliminary studies demonstrated beneficial effects of dietary creatine across different post-viral fatigue syndromes. Creatine is often co-administered with glucose to improve its potency yet whether glucose boost the efficacy of creatine in long COVID remains currently unknown. In this report, we investigate the effects of 8-wk creatine intake with and without glucose on patient-reported outcomes, exercise tolerance, and tissue creatine levels in patients with long COVID. Fifteen male and female long COVID adult patients (age 39.7±16.0 y; 9 women) with moderate fatigue and at least one of additional long COVID-related symptoms volunteered to participate in this randomized controlled parallel-group interventional trial. All patients were allocated in a double-blind parallel-group design (1 : 1 : 1) to receive creatine (8 g of creatine monohydrate per day), a mixture of creatine and glucose (8 g of creatine monohydrate and 3 g of glucose per day), or placebo (3 g of glucose per day) t.i.d. during an 8-wk intervention interval. Two-way ANOVA with repeated measures (treatment vs. time interaction) revealed significant differences in changes in total creatine levels between the groups, showing an interaction effect at two brain locations (right precentral white matter F=34.740, p=0.008; partial η2=0.72; left paracentral grey matter F=19.243, p=0.019; partial η2=0.88), with creatine and creatine-glucose outcompeted placebo to elevate creatine levels at these two locations. Several long COVID symptoms (including body aches, breathing problems, difficulties concentrating, headache, and general malaise) were significantly reduced in creatine-glucose group at 8-wk follow-up (p≤0.05); the effect sizes for reducing body aches, difficulties concentrating, and headache were 1.33, 0.80, and 1.12, respectively, suggesting a large effect of creatine-glucose mixture for these outcomes. Our preliminary findings suggest that supplying exogenous creatine with glucose could be recommended as an effective procedure in replenishing brain creatine pool and alleviating long COVID features in this prevalent condition.
In the study above, many of the Long Covid symptoms such as body aches (muscle pain because of poor blood flow and poor energy turnover and oxygenation), and neurological symptoms improved quite significantly by taking 8 grams of Creatine + 3 grams of Glucose per day.
A little above my suggested dosage, not outside the norm, and very simple, easy to test, and easy to do. Just a reminder that your body can’t absorb amino-acid supplements (powders) really fast, so take only the creatine and wait 3-4 hours to add any other amino-acid-based supplements, so you just don’t waste away part of your supplements and absorb as much as possible.
I will see if I can finish and publish my Genocidal Organ article by Sunday or Monday at the latest, either to convince some of you to watch it, or for anyone to understand its importance from my perspective.
I am grateful for your continued support.





I wish everyone a great weekend. May it be not that eventful =P.
I read the linked study on micro vascular complications and I’d like to point out one interesting fact and one huge issue in the study.
Interesting fact: all of the studied participants had first-wave COVID. In my social circle I knew four people who had first-wave COVID and two were hospitalized and near-death before slow recovery. Every person I know who caught COVID after the first wave, myself included, had relatively-mild flu-like symptoms. The virus went from “wicked bad” to “just the flu” in just one season of mutations. One wonders if later variants had the same micro vascular effects.
One huge issue: the authors tested the subjects two and a half years (31 months) after their acute COVID illness, yet their study provided no information on vaxx status of the patients. In the 31 months after the first wave, vaxxes and boosters were widely available and encouraged, though in Sweden they were not mandated.
We don’t know how many got vaccinated, which vaccine(s) they received, nor do we have booster shot(s) status. This is very important and should have been included in the study parameters. Consider two extreme example possibilities:
One: half refused to get vaxxed and relied on natural immunity against further infections and half got fully vaxxed and took every seasonal booster available. The vaxxed and boosted all have micro vascular complications and the unvaxxed have none. The vaxxes and boosters are long-term harmful!!!
Two: same setup, but the unvaxxed all have the micro vascular complications and the vaxxed and boosted have none. The vaxxes and boosters are awesome and save lives!!!
I believe the majority of the COVID studies intentionally ignore vaccinations as potentially causal. The grant money (by and large) comes from Pharma. Smart people don’t bite the hand that feeds them. Without providing vaccination and booster status the study, sadly, tells us nothing about Covid infections.
Oh, one other issue. The study does not report how many had additional bouts of Covid. In my social circle the group not people I know who have had multiple Covid infections were at least “fully” vaxxed (I.e., two shots of either Moderna or Pfizer).