Yesterday, one of my readers (Shirl3y) shared an interesting paper with me, so I decided to write a short, to-the-point article.
Post coronavirus-disease-vaccination immune reconstitution inflammatory syndrome in tuberculosis treatment: a case report
A 47-year-old Indian man with no past medical history from India developed pain and weakness in his inter-phalangeal and metacarpal-phalangeal joints. On the basis of his symptoms, laboratory testing, and imaging of his hands, he was diagnosed with seronegative rheumatoid arthritis. He was started on biologic treatment with anti-TNF agent adalimumab and methotrexate. Before starting treatment, he had a chest X-ray, which was normal and a test for M. tuberculosis using an interferon gamma release assay, which was also negative. He received two doses of Pfizer mRNA vaccine 4 weeks apart without any complications. Then, 6 months after starting adalimumab, he developed constitutional symptoms including headaches, nocturnal sweats, and low-grade fever. He then developed neck pain and was noted to have bilateral cervical adenopathy noted on exam. Computed tomography (CT) scan of the neck confirmed bilateral cervical adenopathy (Fig. 1). His immunosuppressive therapy was stopped. A cervical lymph node biopsy was performed. The histology results were strongly positive for acid-fast bacilli. A diagnosis of tuberculous lymphadenitis was made, and he was started on a four-drug regimen with Isoniazid, Rifampin, Pyrazinamide and Ethambutol. Within 5 days of starting the regimen, he noted a significant improvement in his symptoms. The mycobacterial cultures revealed that the bacillus was susceptible to all the antituberculous drugs. About 2 weeks after starting his antitubercular therapy, he received a dose of previously scheduled COVID mRNA vaccine (third dose of Pfizer mRNA), and 5 days after receiving the vaccine, he developed severe constitutional symptoms including fever, chills, and excessive diaphoresis. He was admitted to the hospital for further evaluation. His exam was unremarkable for any new finding. He was ruled out for sepsis with negative blood cultures and serological testing. Inflammatory markers including ESR and C-reactive protein (CRP) were elevated at 35 mm/hour and 5.33 mg/l. He was diagnosed with antitumor-necrosis-factor-alpha-induced tuberculosis-associated IRIS. Treatment was started with intravenous methylprednisolone 80 mg every 8 hours, with resolution of his symptoms. He was transitioned to oral prednisolone 100 mg twice a day and discharged home 5 days later. His oral steroids were gradually weaned off over the next 3 months. He finished a 12-month course of antitubercular therapy. He had no recurrent symptoms at 18-month follow-up and was discharged from the infectious disease clinic. He was able to resume therapy with adalimumab after 4 months of antitubercular therapy.
This is a fairly complex patient, without an extensive presentation of the medical history, with seronegative rheumatoid arthritis, a form of RA that has its most common diagnostic tests coming back negative. His treatment involved Humira, a widely used monoclonal antibody with some rather peculiar long-term side effects (it is still useful though, personally, I just am not a fan of monoclonal, which is like the best therapy style for pharma because it is a revolving door style).
So what happened ? There is a significant (>90%) likelihood this patient had latent tubercolosis infection, which remained in check for most if not his entire life since he was first exposed. Humira's primary mode of action is inhibiting a very important part of the immune system, TNF-α. This protein is critical for containing and keeping M. Tuberculosis in check.
On average, it would take 6 months for Humira to impair macrophage and T-Cell function enough to get out of latency, thus the patient experiencing dissemenation to the lymph nodes. Stopping Humira’s treatment enabled the body to recover from its impairment and increased T-Cell count and function. This was likely the worst timing to get the mRNA vaccine.
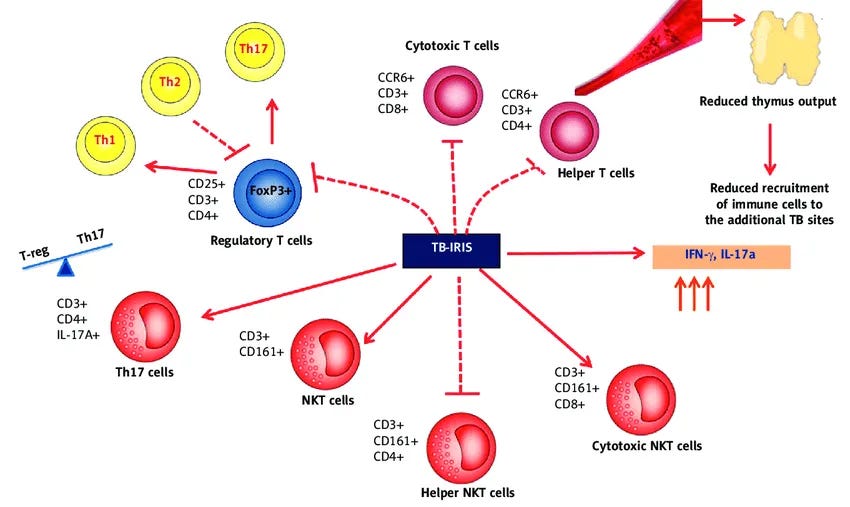
Pfizer’s mRNA, and also Moderna's, are known to have a profound Th1 and especially Th17 response, with abundant production of IFN-γ, IL-6, and TNF-α production, the booster amplified the already active immune response against Tuberculosis. The booster acted as a significant enhancer of an already increasing immune response, creating more than one feedback loop, leading to IRIS. IRIS is an immune-mediated hyper-inflammatory response that occurs in response to specific pathogens whenever your body is recovering its immune cells to normal levels.
Central to my main thesis, lies this tilted, paradoxical immune response, with a profound production of specific inflammatory proteins, and “forcing” the body into a highly inflammatory immune state dominated by Th17 immune cells. Below is a list of pathogens that induce IRIS, which you will instantly find curious (the images and quote below are excerpts from the my article above).
IRIS may occur at any stage in the progression of immunodeficiency and manifests with weakened immune system. IRIS is associated with various inflammatory processes as the outcome of immunological reaction against a variety of opportunistic infections (OIs).
As with everything, with more research, deeper understanding, and more time, you come to develop a nuanced perspective on everything. IRIS, per the medical definition, will remain exceedingly rare, but cases will increase slowly, but surely, yet per this brief overview, you understand how many factors must be occurring at the exact same time for the hyper-inflammatory response to kick in.
So why didn’t IRIS happen at a large scale after years ? Simply put, the body possesses multiple intrinsic mechanisms and self-initiating feedback loops to avoid hyperinflammatory states. The significant apoptosis (cell death) alone, observed at the first 4 weeks of the mRNA vaccine, will protect the body. Significant higher production of cortisol will do the same (although this may cause adrenal failure in some unlucky few). Modulating the cell’s own receptors in response to all this.
Since IRIS takes months to develop, per the gradual recovery of immune cells and an absurd response towards a secondary, opportunistic pathogen, what avoiding IRIS via multiple mechanisms did was leave the doors open towards new infections. This starts a months-long cycle of infections, constantly being sick, but not severely sick. So infections start lasting longer, behaving differently, and taxing the body more, but you avoid the severe immunological storm.
The bone marrow carries the heaviest burden (the next article, which will be long and complex). At some point in the near future I will rework my PAID hypothesis and write a properly written proposition and not an amalgamation of complex information and hints.
I appreciate your support, it enables my long journey into the depths of data.







I find these case reports increasingly difficult to assess when the dates of illness and treatment are excluded.
"Third dose of mRNA" implies 2022, we have no indication of his previous Covid serology (and I was not hoping for a PCR report!)
Although the patient was reported as Indian the report was from Texas and Louisiana. By 2022 the problems with the mRNA shots were well known in India.
It would have been interesting to know his RA response to the prednisolone dosage apart from the adalimumab.
Interesting case, thank you.
"...in the near future I will rework my PAID hypothesis and write a properly written proposition..."
Excellent! Much looking fwd to it!!