How brain fluid dynamics link sleep, focus, and neurological decline
Attention Lapses, Glymphatic Flow, and Dementia
As I deal with things, this will be another one of the series of shorter analyses that go straight to the point and lack an “overall theme”. Albeit, I will try to maintain an overall theme in this one.
By sheer coincidence, I just experienced an extended period of sleep loss, and like most people, this significantly affects my focus, which I can “out run” in bursts, but it taxes the body and mind in a sense. Improper sleep is very damaging to the body, with the effects mostly showing themselves over extended periods of sleep loss, but there is a common, experienced by anyone, short-term effect. Loss of focus.
Is the lack of focus a lack of proper energy metabolism ? Lack of rest ? Well, we shall wonder no more. In line with a topic I have an interest in. The Glymphatic System.
Over time, we learned how the glymphatic system works in the body, by using certain neurotransmitters to create steady pulses while you sleep, to quite literally, use fluid to flush out bad proteins, thus, this creates multiple mechanisms that can be disrupted. Poor vascular flow, vascular health will impact this, and so the fluctuation or disruption of certain neurotransmitters and their production.
Attentional failures after sleep deprivation are locked to joint neurovascular, pupil and cerebrospinal fluid flow dynamics
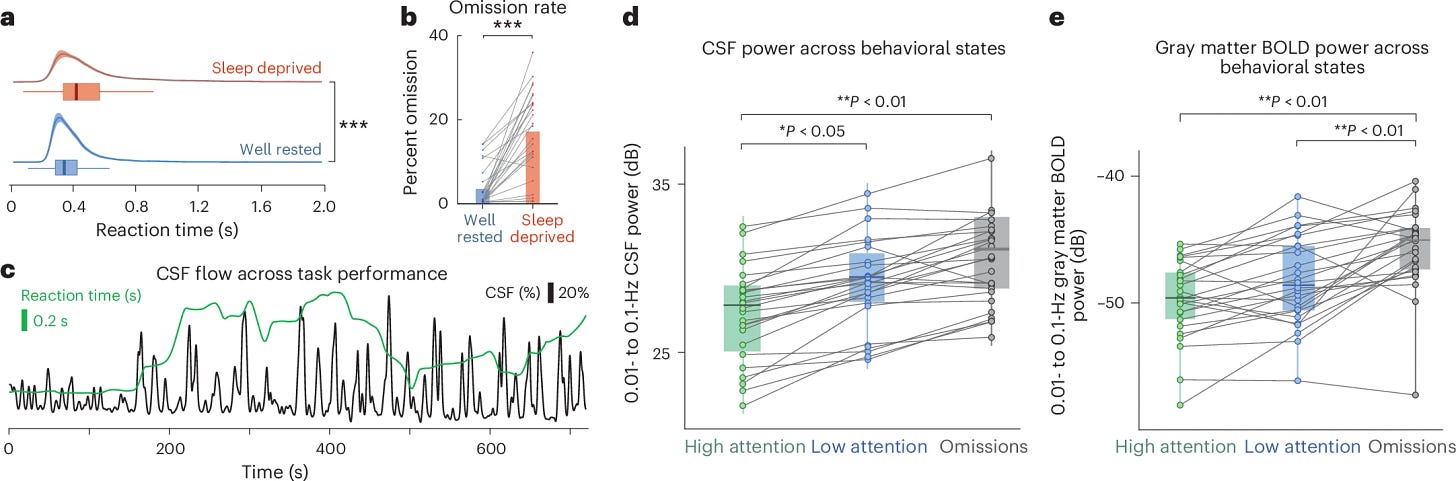
As with good modern research, the researchers used a multimodal approach, using different testing and methods to observe changes in the patients. The approach here is a “within-subject”, the 26 patients were scanned on two distinct occasions, after a normal night of sleep (well-rested) and after a full night of total sleep deprivation. The tests were EEG (measures the electric activity in the brain), and fMRI (measures the flow of blood, mostly), and these were simultaneous tests for a more comprehensive approach.
Inside the MRI machine, there is an eye-tracker, and pupil size is an excellent, real-time proxy for brain activity, especially the noradrenergic system, the neuron network responsible for producing norepinephrine (noradrenaline), important later on.
Upon investigating whether sleep deprivation altered the flow of CSF (cerebrospinal fluid), first the authors saw that when well-rested (normal sleep), parcipants waking CSF flow was normal, with rapid oscillations tied to breathing. But upon being sleep deprived, the researchers observed the emergence of large-amplitude, low-frequency waves in the CSF signal. These waves are signature waves for NREM sleep, but they were awake.
This finding was also observed in brain oxygenation (BOLD signal fluctuations) and in changes in EEG frequency. They then tested whether these large fluid waves impacted attention, given that attention is highly suppressed during sleep. Low-frequency CSF and BOLD waves were significantly higher during low attention moments, and highest of all during omissions, tying the sleep-like fluid dynamics to the attention failure.
An important aspect of this part of the test was using the pupil size/dilation. Important because it ties the noradrenergic system with the changes, which in turn ties the fluid dynamics changes with vasculature changes. These changes are reflected systemically.
There is an initial change in the neural and electrical activity in he brain, followed by a heart rate and respiratory rate dip, and a biphasic event occurs. First, CSF flows outward from the brain, and this is followed by a recovery process where it flows back inward. This cascade of events creates attention failure.
How it works ?
Sleep deprivation makes the Locus Coeruleus, a part of the brain responsible for, among other things, the synthesis of norepinephrine, become unstable. This initiates a cascade of events. Norepinephrine is essential for maintaining alertness, among many, many other neurological effects, such as memory formation, learning, and another important effect.
A drop in the neurotransmitter leads to changes in electrical activity in the brain, and impairs neural processing. Noradrenaline (also known as Norepinephrine) is a potent vasoconstrictor (it narrows blood vessels), a drop causes the blood vessels to dilate. This widespread vasodilation causes a large, slow increase in cerebral blood volume, acting as a mechanism to push CSF outward (out of the skull space).
The brain picks up on this lapse and triggers a response, releasing a surge of norepinephrine, causing widepread vasconscritcion, squeezing blood out of the brain, creating space for CSF to be drawn back inward. This matters a lot. In my article linked above, one of the articles inside is how Norepinephrine controls the glymphatic system flows, creating pulses that control the vasculature and are a key part of the waste removal.
Under a sleep-deprived, yet awakened state, the body will still activate the glymphatic system under specific events, to clean itself, at the cost of momentarily losing focus (attention failure). Staying within the theme, let us cover 3 interesting papers. Lack of sleep affecting focus, affecting neurological health, is one thing, but could sound affect focus and memory too ?
Environmental sounds impact memory: Effects of city-related and nature-related sounds on episodic memory
In this foundational work, we observed evidence that city-related sound exposure had a negative impact on episodic memory as measured by context memory. This finding adds to decades of research that has shown a constellation of harms to city-related sound exposure on both health and cognition. Given the importance of episodic memory abilities for daily function, the current findings suggest a new type of harm attributable to exposure to city-related sounds (e.g., reduced context memory). We did not find any evidence of improved episodic memory under nature-related sound exposure conditions, but more work may be necessary to better understand how nature-related sound exposure might affect other aspects of cognition, including memory. In contemporary times, people increasingly live in urban environments, and so it is imperative to better understand how aspects of modernity (e.g., city-living) affect well-being and cognitive health. The findings of the current investigation, along with decades of prior work across many scientific disciplines, underscore the importance of increased understanding of how factors associated with daily living, like city-related sounds, affect aspects of cognition, particularly memory.
The authors cite substantial prior evidence, and did extensive research on adding to the evidence of the negative impacts of environmental, city noises on memory, which negatively impacts the brain. A 2024 study demonstrated that low-frequency noise can negatively impact higher-order cognitive functions, such as logical reasoning, mathematics, and data processing. In this meta-analysis, the authors found evidence that noise exposure may negatively impact cognitive function in children and adolescents.
I suspect these can contribute to dysfunction over a necessarily long timeline (decades). There is a huge discussion on social media on the effects of wireless frequency on human health, but it is the second time in this Substack that I recommend noise-cancelling headphones. These are the best purchases I have made for my attention, focus, and overall productivity, anything that blocks outside noise and distraction. And noise, and specific sounds clearly have a negative cognitive impact.
MRI markers of cerebrospinal fluid dynamics predict dementia and mediate the impact of cardiovascular risk
INTRODUCTION
Impaired cerebrospinal fluid (CSF) dynamics may contribute to dementia, but human evidence is limited. We examined associations between magnetic resonance imaging–based proxies of CSF dynamics and incident dementia, and whether CSF dysfunction mediates links between cardiovascular risk and dementia.
METHODS
Using the UK Biobank, we measured CSF dynamics: perivascular space (PVS) volume, diffusion tensor image analysis along the PVS (DTI-ALPS), blood oxygen level–dependent CSF (BOLD-CSF) coupling, and choroid plexus (CP) volume. We assessed cardiovascular risk factors and their associations with CSF dynamics and dementia based on general practitioner, mortality, and hospital records. Mediation analysis evaluated CSF dysfunction in cardiovascular risk–dementia relationships.
RESULTS
Lower DTI-ALPS, lower BOLD-CSF coupling, and higher CP volume predicted dementia, but PVS volume did not. DTI-ALPS and CP volume mediated the effect of white matter hyperintensities and diabetes duration on dementia.
DISCUSSION
Impaired CSF dynamics may lead to dementia and partially mediate cardiovascular risk–dementia associations.
Highlights
We developed fully automated methods for quantifying diffusion tensor image analysis along the perivascular space (DTI-ALPS) and blood oxygen level–dependent cerebrospinal fluid (BOLD-CSF) coupling.
Three CSF dynamics markers—BOLD-CSF coupling, DTI-ALPS, and choroid plexus (CP) volume—were predictive of incident dementia, whereas PVS volume was not.
Magnetic resonance imaging proxies of CSF dynamics markers were associated with cardiovascular injury. CP volume and DTI-ALPS mediated the associations of both white matter hyperintensities and diabetes with dementia.
The UK Biobank is a massive medical database, with tons of data, and, significant to this paper, imaging data from tens of thousands of people. With such a large amount of data, you can find patterns to deduce or actively propose specific dynamics, especially over time.
They created and used multiple automated and deep-learning algorithm approaches to go through the data, classify, and find such patterns. They use 4 specific ways to measure CSF dynamics and their association with long-term dementia risk and how cardiovascular health affects this.
BOLD-CSF coupling, directing the measurement of blood flow and oxygenation, and CSF flow. Cpuling means more efficient pumping. DTI-ALPS, if you remember, a way to measure how easily water moves along the perivascular space, where CSF flows, higehr DTI-ALPS means better, faster movement and clearance. Choroid Plexus volume, CP is the tissue responsible for producing CSF.
Swollen or enlarged CP means dysfunctional CSF production and waste clearance. Perivascular Space Volume (PVS), the channels the fluid travels themselves. Enlarged PVS = fluid stagnation, slow removal. Closely to what they found in the data, where lower BOLD-CSF coupling predicted higher risk of dementia, lower DIT-ALPS predicted higher risk of dementia, and higher CP volume predicted higher risk of dementia.
Next, they found an association between markers of cardiac and arterial function, especially risk factors such as diabetes, high blood pressure, and arterial stiffness were directly associated with worse CSF flow/dynamics. Interestingly enough, in this cardiac marker section, the strongest marker was WHM, White Matter Hypersensitivity.
This is a way to measure and observe small vessel, ergo the microvasculature, dysfunction in the brain. The authors argue that small vessel (WMH) is the endpoint of cerebrovascular injury, impacting and lowering the driving force of CSF and contributing to cognitive decline. I would argue it is both. Start and end point, primary small vessel damage, and systemic endothelial damage, such as from Covid will initiate a cascade of events, and this creates a feedback loop leading to the progression of dementia.
The last paper is similar in fashion to the latter, where they used data from the UK Biobank, from 27.500 adults.
Poor sleep health is associated with older brain age: the role of systemic inflammation
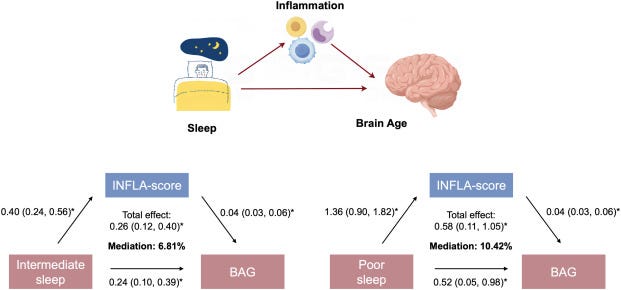
The study included 27,500 adults from the UK Biobank (mean age 54.7 y, 54.0% female). The presence of five self-reported healthy sleep characteristics (early chronotype, 7–8 h daily sleep, no insomnia, no snoring, no excessive daytime sleepiness) were summed into a healthy sleep score (0–5 pts) and used to define three sleep patterns: healthy (≥4 pts), intermediate (2–3 pts), and poor (≤1 pt). Low-grade inflammation was estimated using the INFLA-score, a composite index of inflammatory biomarkers. After a mean follow-up of 8.9 y, brain age was estimated using a machine learning model based on 1079 brain MRI phenotypes and used to calculate brain age gap (BAG; i.e., brain age minus chronological age). Data were analysed using linear regression and generalised structural equation models.
Findings
At baseline, 898 (3.3%) participants had poor sleep, 15,283 (55.6%) had intermediate sleep, and 11,319 (41.2%) had healthy sleep. Compared to healthy sleep, intermediate (β = 0.25 [0.11, 0.40], P = 0.010) and poor (β = 0.46 [0.05, 0.87], P < 0.001) sleep were associated with significantly higher BAG. In mediation analysis, INFLA-score mediated 6.81% and 10.42% of the associations between intermediate and poor sleep and higher BAG.
Interpretation
Poor sleep health may accelerate brain ageing. This may be driven by higher levels of systemic inflammation.
Sleep disturbances are becoming widespread and far too common, both from geopolitical influences to economics, and of course, a lasting byproduct of the pandemic. It has been known for years that poor sleep affects your overall health, from your immune system to your organs, leading inevitably to neurological issues over time.
The evidence backs the author’s proposition, poor sleep increases systemic, low-grade inflammation, which in turn shifts the systemic metabolism, from an organ to a cellular level, and over time it accelerates brain aging. This is why people with insomnia or sleep apnea have measurable older brains than healthy individuals. Albeit there is many pathways leading to these, there are 3 distinct mechanisms of interest here.
The dopaminergic pathway, the noradrenergic pathway, both share a common biosynthetic pathway, and certain functions, possessing mutual influence and can be released at the same time, and the Kynurenine pathway. The first two are damaged, especially over the long term by SARS-CoV-2, and the last one is imprinted for months. One of my goals soon is to dissect these pathways, given the recent evidence and circumstances.
I am thankful for your support.




First, thank you to the people who donated and the recent paid subscribers. God willing I will soon have my PC situation figured out.
After that, I will be able to achieve higher productivity because my workflow can be resumed and enhanced.
Thus the question. There are a lot of papers to cover. Do you want a comprehensive layered analysis. Or single ones (often covering one single paper).
Readers choice here.
I hope you all have a great weekend.
Great article to read, especially at (checks notes) …4 a.m.
The brain fog, aging, poor sleep, inflammation and circulation are reparable, at least some damage is reversible.
Western “medicine” poisons. Other than going for repairs (stitches, broken bones). Any jabcine causes horrendous damage, sleep disturbances, inflammation, toxic overload, immune system compromise. Avoid tetanus, flu, etc. Avoid doctors, RNs, LNPs. Go light on alcohol, sugar and late night snacks.
Find good, organic farmers, get to know them, eat raw foods, raw milk and yogurt.
Get a sleep study. You may need years of good rest and a CPAP machine. Even mouth Tape and a chin strap can help.
Be sure to have a good bed that doesn’t hurt your back, Japanese few inches of padding on the floor, knees supported or slightly elevated may help. Shoulders must be flat on bed/ floor and only head and neck on pillow. You should be able to lift either corner of the pillow and clear your shoulders. Another pillow can go under the knees or between them.
I haven’t narrowed down which one, but reishi, ashwaganda, cordyceps + shiitake , rhodiola and lion’s mane have been GAME CHANGERS for getting back:
- daily clarity
- focus to study
- after lunch energy
- lack of headache in pm after intense work
Avoid MSM, too much screen time, cults, hunching over and engaging with toxic people.
Get your blood flow up, laugh, spend time with quality people, in prayer, meditation and reflection. Talk to God.