As I wrote shortly ago, I would keep everyone updated on the Congolese mystery, but I will also add a few interesting papers, so you can see this as an AIDA, a round-up of interesting things that don’t fit one theme.
As I suspected, “Disease X”, which I don’t know why the entire media converged into naming the Congolese disease as that within 24 hours of each other, was one of the most common epidemics in the region and throughout Africa. Malaria.
Congo's health ministry says unknown disease is severe malaria
Democratic Republic of the Congo, Dec 17 (Reuters) - Democratic Republic of Congo's health ministry said on Tuesday that a previously unidentified disease circulating in the country's Panzi health zone is a severe form of malaria.
Earlier this month, local authorities said the disease had killed 143 people in the southwestern Kwango province in November.
"The mystery has finally been solved. It's a case of severe malaria in the form of a respiratory illness... and weakened by malnutrition," the health ministry said in a statement.
It also said that 592 cases had been reported since October with a fatality rate of 6.2%.
As I suspected, malnutrition plays a considerable role when taking into account “mysterious outbreaks” in many regions of the world. Either some “immunological shift” by known causes or malnutrition. Now, how they attribute “respiratory transmission” to a mosquito-borne disease known to have pulmonary manifestation, is being me. Alas, another mystery solved.
Given my focus on the brain, neurological health, neurological enhancements, and overall anything related to “neuro”. An egg a day keeps Alzheimer’s away.
Results
This study included 1024 older adults {mean [±standard deviation (SD)] age = 81.38 ± 7.20 y}. Over a mean (±SD) follow-up of 6.7 ± 4.8 y, 280 participants (27.3%) were clinically diagnosed with Alzheimer’s dementia. Weekly consumption of >1 egg/wk (hazard ratio [HR]: 0.53; 95% confidence interval [CI]: 0.34, 0.83) and ≥2 eggs/wk (HR: 0.53; 95% CI: 0.35, 0.81) was associated with a decreased risk of Alzheimer’s dementia. Subgroup analysis of brain autopsies from 578 deceased participants showed that intakes of >1 egg/wk (HR: 0.51; 95% CI: 0.35, 0.76) and ≥2 eggs/wk (HR: 0.62; 95% CI: 0.44, 0.90) were associated with a lower risk of AD pathology in the brain. Mediation analysis showed that 39% of the total effect of egg intake on incident Alzheimer’s dementia was mediated through dietary choline.
Conclusions
These findings suggest that frequent egg consumption is associated with a lower risk of Alzheimer’s dementia and AD pathology, and the association with Alzheimer’s dementia is partially mediated through dietary choline.
I am a big proponent of daily egg consumption because it is one of the best “super-foods” there is, outside liver (which I can’t stand eating), and other studies have consistently demonstrated that egg consumption lowers the incidence and lowers the risk of developing Alzheimer’s and similar neurodegenerative disorders. Eggs are rich in Choline, which is one of the most important nutrients in regard to your nervous system, your neurological function, and health, and even act as a direct systemic anti-inflammatory nutrient by activating the CAP (Cholinergic Anti-inflammatory pathway).
Just a few eggs per week have long-term benefits, but there isn’t exactly a limit on daily egg consumption, the “trick” is avoiding higher egg consumption with high carbohydrate diets. Even if you consume eggs I am still a big proponent of Choline (+Inositol) supplementation, because no matter how much eggs you consume, we are eternally limited by nutritional vs therapeutic levels of any nutrients. Consuming food = nutritional levels. Supplementation = therapeutic. There is a place and time for both.
Given the subject of my last article where I cited the quite important and significant role NR4A1 plays, although paradoxical many times, here is a fascinating new paper.
Systematic review: Orphan nuclear receptor subfamily 4 group A (NR4A in human and Nr4a in rodent) contains three immediate early genes, Nr4a1, Nr4a2, and Nr4a3. The brain expressions of rodent Nr4a increase quickly after learning activities. Expressing the dominant-negative Nr4a form (Nr4aDN) or repressing Nr4a by HDAC3 leads to impaired contextual fear memory in rodent, demonstrating the critical role of Nr4a in cognition. Blocking Nr4a impairs the later phase of long-term potentiation, which is considered as a cellular basis of learning and memory, indicating that Nr4a contributes to the gene expression period of synaptic plasticity. A recent study shows that the immediate expression increment of Nr4a1/2 after learning activity is deficient in aged mice with cognitive impairment, and transcriptomic study indicates that Nr4a1 is decreased in aged mouse brain. However, the pattern of reduction of Nr4a1 expression is unclear, and the cause of Nr4a1 reduction and cognitive decline with aging remains elusive.
Interpretation: NR4A1/Nr4a1 was reduced in the peripheral blood mononuclear cells in both aged humans and mice, and was severe in aged individuals with cognitive disorders. In addition, we demonstrated that Nr4a1, but not Nr4a2/3, was specifically decreased in the mouse hippocampal CA1 region and cortex. NR4A1 also declined with aging in the human hippocampus. We found that Nr4a1 ablation impaired the dendritic spine density and glutamate receptor expression in CA1, and led to synaptic dysfunction and cognitive injury. Overexpressing Nr4a1 in CA1 pyramidal neurons improved the cognition of aged mice. Intriguingly, Nr4a1/NR4A1 directly bound to TrkB promoter in both mouse and human genomic backgrounds, and induced the transcriptional activity of TrkB, which was necessary for Nr4a1-dependent cognitive enhancement.
Many months ago, when talking about misfolded proteins and their rather highly complex role in human health and disease, I wrote that older people with neurodegeneration often don’t suffer, or have a significantly lower burden of cancer, than other groups. Here there is more evidence for it. Lower levels of NR4A1 as we age, or during other conditions will inevitably cause worsening and decline of cognitive health. But as a paradoxical byproduct, it also lowers your chance of developing many types of cancer. A rather bitter choice. Lose your mind, or lose your body…
And lastly today, a paper I would advise everyone to read. Yes, the entire thing.
The metabolic role of vitamin D in children’s neurodevelopment: a network study
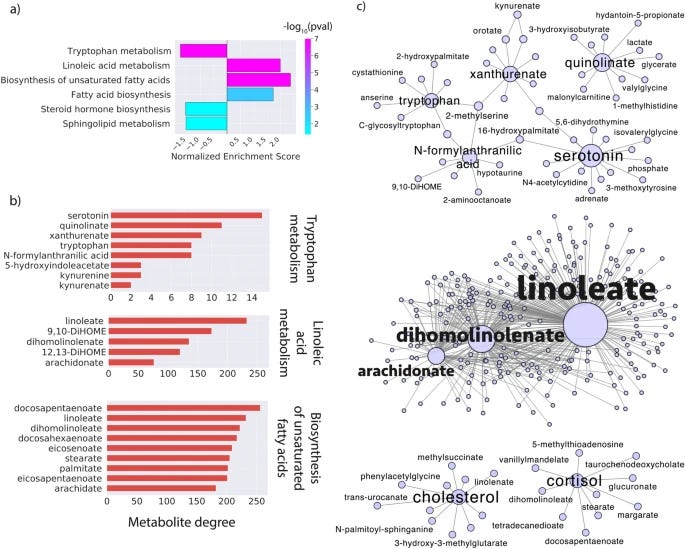
As I have written a few times throughout the years, Vitamin D is not merely a nutrient, or “vitamin”, but it is a regulatory hormone ruling over too many biological processes to list. A overlooked function, until now, is its involvement in modulating tryptophan metabolism, where tryptophan is converted into serotonin and kynurenine.
In ASD individuals, research has consistently found elevated levels of kynurenine and its metabolites in the blood of the patients in these studies, and many of these metabolites are neurotoxic and can incentivize neuroinflammation and neuronal damage. Low Vitamin D will incentivize a loop of dysfunction in the Tryptophan metabolism towards the Kynurenine pathway, creating an inflammatory loop that affects everything, cognition, mood, immune system, neural plasticity, and the list goes on.
Here the authors found statistically significant associations between the levels of Vitamin D in children and their mothers both during and after pregnancy and how it affects the neurodevelopment of the children.
Vitamin D Interaction map, an analysis of where Vitamin D may interact, influence or directly affect different amino acids, fatty acids, or hormones. The main ones in the Tryptophan Pathway were serotonin, quinolinate, xanthurenate, and kynurenine, already levels of these influence depression, overall neurological health, ADHD, and ASD.
Linoleate, dihomolinolenate and arachidonate are part of the Linoleic Acid Metabolism and also Fatty Acid biosynthesis pathway, deficiency in these has been observed in many forms of learning disabilities and ASD. There is also a deficit in producing cholesterol. Deficiency in Vitamin D will affect all these pathways, which will affect dozens of other metabolites, and biochemical pathways.
As a point of observation, aberrant fatty acid metabolism, such as observed here, is often observed in many patients that survive severe Covid infection or have neurological sequelae.
Per its double-edge nature, the Kynurenine Pathway is once again one in the context of this paper. While some of its metabolites, such as kynurenic acid, are neuroprotective, others, like quinolinic acid, are neurotoxic as I have explained before. The VDI network demonstrates that vitamin D deficiency skews this balance, amplifying the production of neurotoxic metabolites and exacerbating risks for neurodevelopmental disorders, and since the KP and its metabolites are also immunomodulatory, changing your entire immune response, they also play a role in that.
By steering tryptophan metabolism toward serotonin synthesis and away from excessive kynurenine pathway activation, Vitamin D is somewhat essential to assuring the body stays on the good side of the Tryptophan metabolism. Per the author’s own observations, large clinical and epidemiological evidence, even when mothers are directed to supplement with Vitamin D, or with the guidance from health organizations, Vitamin D insufficiency and deficiency still plague the world.
Allied to the fact that the widespread infection with SARS-CoV-2 Omicron lineages, and constant bombardment of the body with other pathogens, there is a yet to be recognized, but extremely necessary need to both assess and supplement Vitamin D at all stages of pregnancy and early years of life. Plus many other nutrients. Choline, B vitamins (especially B9, and B12), Creatine (amino acid), and Omega-3 before, during, and after pregnancy all positively affect the long-term health of children. If I had a kid I would set the kid to outpace every single person cognitively and physically =).
Vitamin D attenuates monosodium glutamate-induced behavioural anomalies, metabolic dysregulation, cholinergic impairment, oxidative stress, and astrogliosis in rats
Highlights
MSG impaired long and short-term memory, reduced exploratory behavior, and increased anxiety.
MSG induced dyslipidemia, oxidative stress, lipid peroxidation, altered cholinergic transmission, and neuroinflammation in brain regions.
Vitamin D intervention mitigated the adverse effects of MSG exposure.
Vitamin D exhibits potent antioxidant, anti-inflammatory, and neuromodulatory properties towards MSG-induced neurotoxicity.
An extremely short but pertinent article tomorrow. Perhaps more than one as the year’s end depends on the vibes =P.
I appreciate your continued support, it enables me to continue my independent interdisciplinary research.




I am having fun writing a short-story so I may publish it at New's Year Even. We will see.
I was studying nutrition in the 80s and was lucky enough to be taught by a woman whose mantra was "extraordinary claims require extraordinary evidence" so when the health guidelines solidified into one egg per month max she treated it with the disdain it deserved. The demonization of eggs has been so incredibly damaging to health it makes me furious to contemplate it.